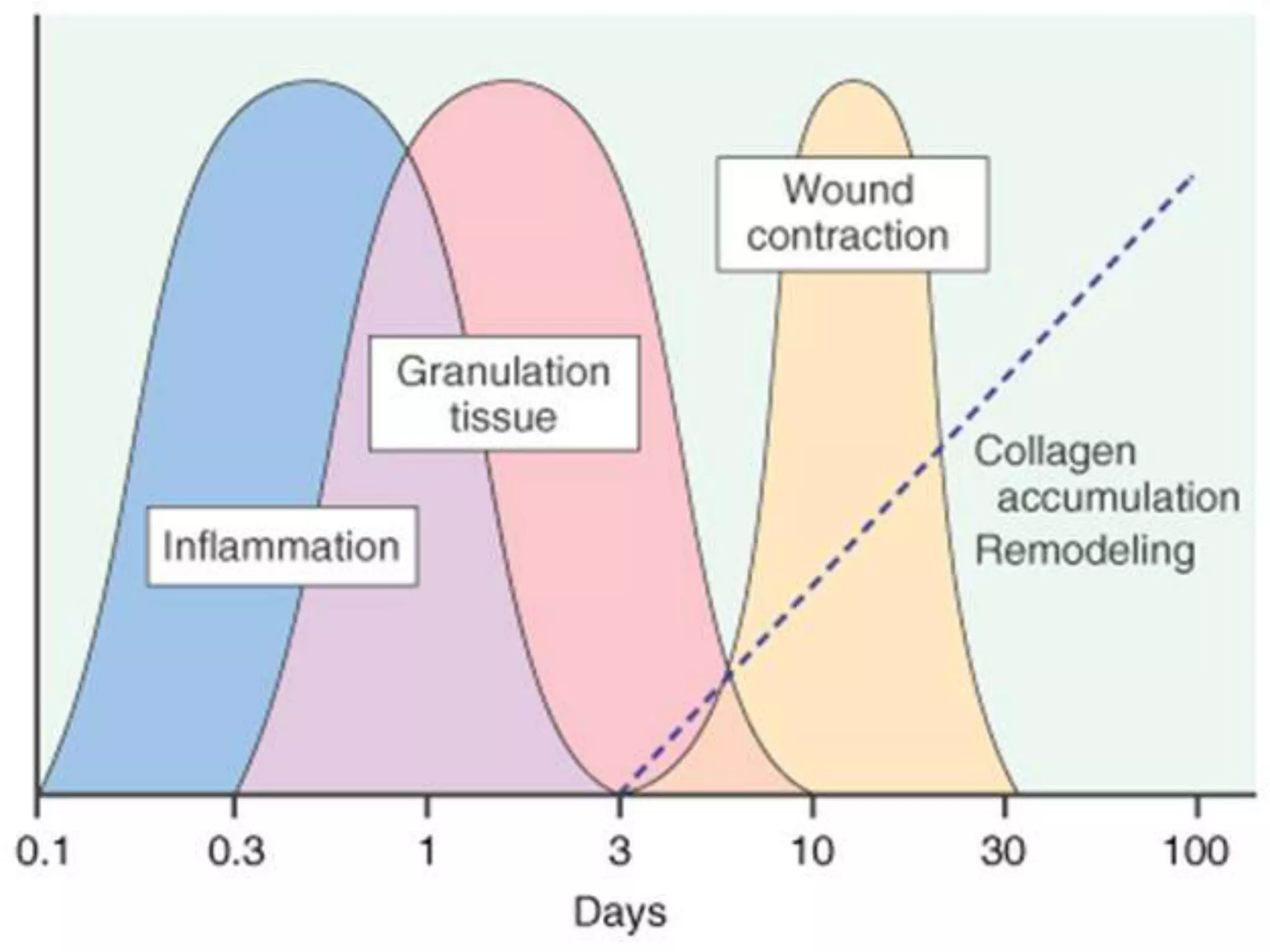
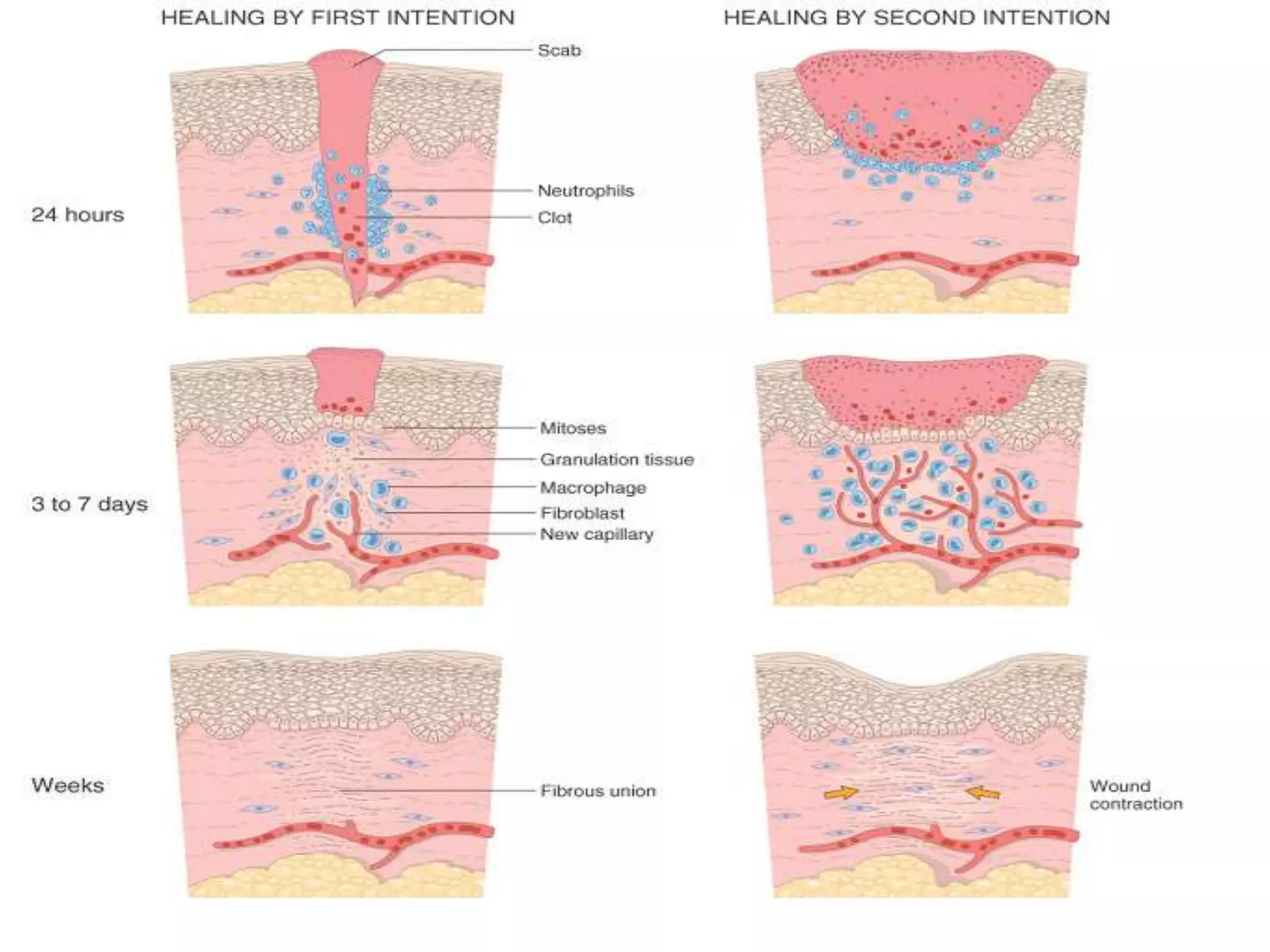
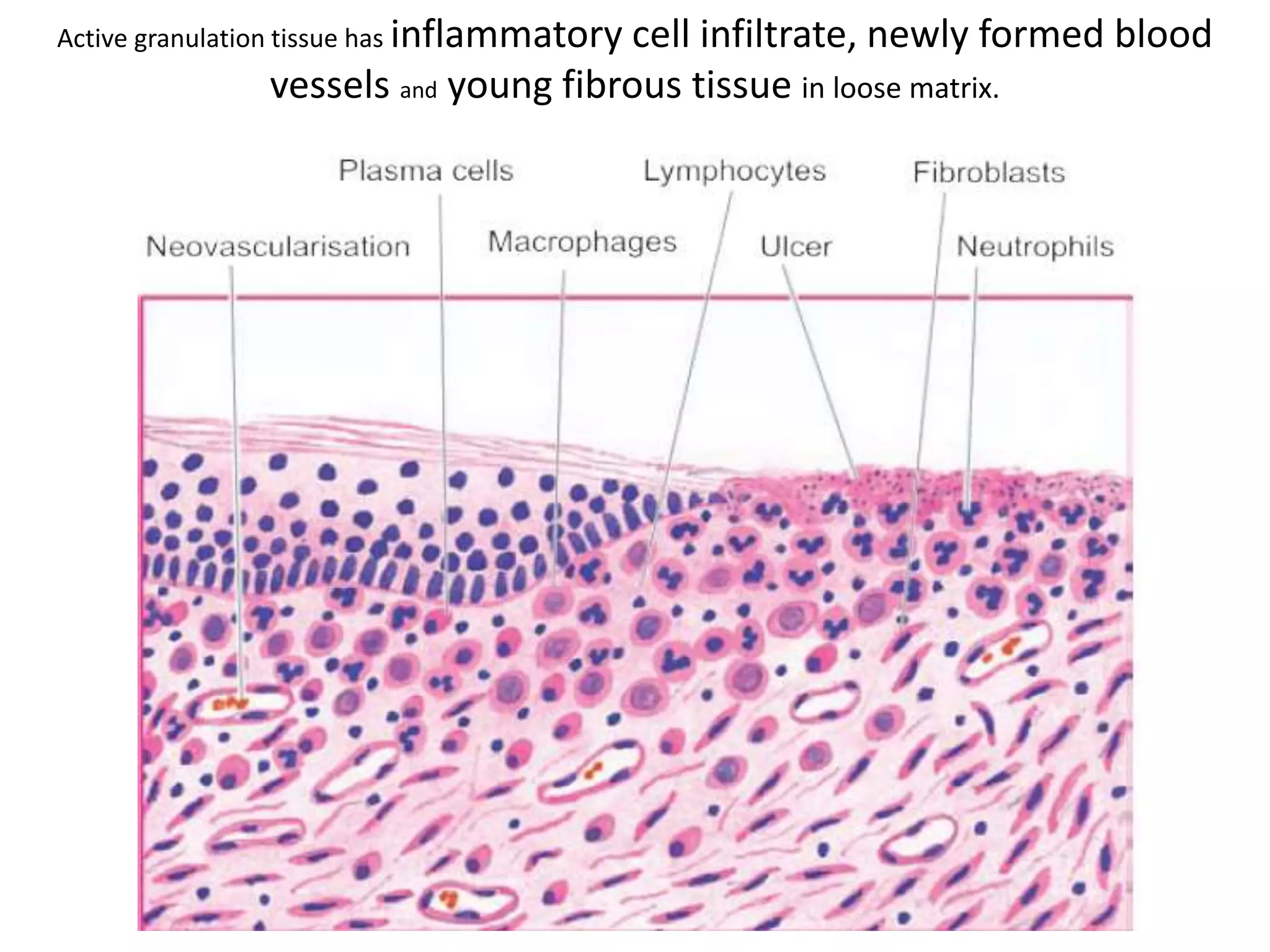
1. Granulation tissue is highly vascularized connective tissue composed of newly formed capillaries, proliferating fibroblasts and residual inflammatory cells. It forms during the healing process to fill wounds.
2. Angiogenesis and fibrogenesis are the two main processes involved in the formation of granulation tissue. Angiogenesis involves the formation of new blood vessels, while fibrogenesis is the formation of new collagen fibers by fibroblasts.
3. Mature granulation tissue consists of a network of thin-walled blood vessels surrounded by fibroblasts in a collagen-rich matrix. It eventually transforms into a vascular scar through further collagen deposition and wound contraction.