Recommended
PPT
MEDICAL CODING FOR HEALTH PROFESSIONALS
PDF
Boost Reimbursements through Professional Medical Coding.pdf
PDF
Accurate Medical Coding Services That Maximize Reimbursements
PDF
Boost Claim Accuracy with Expert Medical Coding Services.pdf
PDF
Accuracy Matters: The Role of Medical Coding Services in Healthcare Compliance
PDF
Medical Coding Best Practices: Avoiding Common Errors
PDF
Navigating Healthcare Codes: Professional Medical Coding Services
PDF
Providers Solutions USA.pdf
PDF
Boost Revenue Cycle Management with Smart Back Office Billing & Coding
PDF
Optimizing Medical Billing and Coding Efficiency
PDF
Medical Coding Courses in Nagpur IIMSkills
PPT
AHLA Basic Coding for Lawyers Presentation
PDF
Current Procedural Terminology
PDF
Medical Coding Audit Services Ensuring Accurate and Compliant Healthcare Codi...
PDF
The Difference Between Medical Billing and Coding.pdf
PDF
Prevent Denials with Precise Medical Coding
PPTX
Introduction to Medical Billing and Insurance
PDF
Common Medical Coding Challenges and How New York Companies Overcome Them.pdf
PPTX
Getting Paid in 2023: Strategies to Maximize Your Revenue
RTF
PPTX
PRINTOUT Exploring the World of Medical Coding (1).pptx
PDF
US Medical Billing A Comprehensive Overview for Healthcare Providers.pdf
DOCX
Common Medical Coding Mistakes and How to Avoid Them.docx
PDF
Healthcare Coding Services Ensuring Accurate Medical Coding Audit Services.pdf
PDF
Medical Coding and Audit Services Unlocking the Potential in Healthcare.pdf
PPTX
2018-09-04-Coding-framesndkbcfdn-CHCF (1)
PPTX
Demystifying Medical Billing and Coding A Comprehensive Guide.pptx
DOCX
Understanding the Vital Role of Medical Billing and Coding
PDF
AI in Healthcare Automating Clinical Documentation to Improve Efficiency and ...
PPTX
ERMP Session for residency candidates- Presentation.pptx
More Related Content
PPT
MEDICAL CODING FOR HEALTH PROFESSIONALS
PDF
Boost Reimbursements through Professional Medical Coding.pdf
PDF
Accurate Medical Coding Services That Maximize Reimbursements
PDF
Boost Claim Accuracy with Expert Medical Coding Services.pdf
PDF
Accuracy Matters: The Role of Medical Coding Services in Healthcare Compliance
PDF
Medical Coding Best Practices: Avoiding Common Errors
PDF
Navigating Healthcare Codes: Professional Medical Coding Services
PDF
Providers Solutions USA.pdf
Similar to Workflow for medical coding process .pptx
PDF
Boost Revenue Cycle Management with Smart Back Office Billing & Coding
PDF
Optimizing Medical Billing and Coding Efficiency
PDF
Medical Coding Courses in Nagpur IIMSkills
PPT
AHLA Basic Coding for Lawyers Presentation
PDF
Current Procedural Terminology
PDF
Medical Coding Audit Services Ensuring Accurate and Compliant Healthcare Codi...
PDF
The Difference Between Medical Billing and Coding.pdf
PDF
Prevent Denials with Precise Medical Coding
PPTX
Introduction to Medical Billing and Insurance
PDF
Common Medical Coding Challenges and How New York Companies Overcome Them.pdf
PPTX
Getting Paid in 2023: Strategies to Maximize Your Revenue
RTF
PPTX
PRINTOUT Exploring the World of Medical Coding (1).pptx
PDF
US Medical Billing A Comprehensive Overview for Healthcare Providers.pdf
DOCX
Common Medical Coding Mistakes and How to Avoid Them.docx
PDF
Healthcare Coding Services Ensuring Accurate Medical Coding Audit Services.pdf
PDF
Medical Coding and Audit Services Unlocking the Potential in Healthcare.pdf
PPTX
2018-09-04-Coding-framesndkbcfdn-CHCF (1)
PPTX
Demystifying Medical Billing and Coding A Comprehensive Guide.pptx
DOCX
Understanding the Vital Role of Medical Billing and Coding
Recently uploaded
PDF
AI in Healthcare Automating Clinical Documentation to Improve Efficiency and ...
PPTX
ERMP Session for residency candidates- Presentation.pptx
PPTX
Outbound Medical Tourism from Bangladesh (2024–2025): A BHA Analysis of the B...
PDF
Advanced Diagnostic Services Offered by the Best Pathology Lab in Mumbai: A C...
PDF
Key Signs of Excellence in Memory Care.pdf
PPTX
Strengthening India’s Oral Health System
PPTX
Marburg virus Orienation_MVD PPT (1).pptx
PPTX
Supraventricular tachycardia presentation.pptx
PPTX
Clinical Audit of Preoperative Preparation in Oral Cancer Surgery as per NCCN...
PPTX
How We Achieved FDA 510(k) Clearance for a Male Latex Condom – Case Study.pptx
PPTX
ISO 13485 Certification Journey- A case Study from I3CGLOBAL.pptx
PPTX
Mgt of endocrine emergencies in ICU.pptx
PDF
Metabolism Myths vs Science: Understanding How Your Body Really Burns Energy
PPTX
General principles of Plaster of Paris cast/slab immobilization in fracture ...
DOCX
Should You Invest in LinkedIn Accounts for Your Outreach Strategy_.docx
PPTX
Common Causes of Lower Abdominal Pain After Sex.pptx
PDF
Ed Strachar- Illuminating the Path to Energetic Freedom with Healing Genius®.pdf
DOCX
Decoupling Care from Campaigns: Jayesh Saini’s Vision for Independent Health ...
PDF
Rangeela Spa Ajman — We Invites You to Enjoy a Calm and Peaceful Experience
PDF
Vascular-Derived Primary Cells: Defining Blood Vessel Tone
Workflow for medical coding process .pptx 1. 2. Introduction
• Objective: To ensure accurate medical coding
for claims processing and compliance.
• Purpose of the Workflow:
• - Minimize coding errors.
• - Optimize revenue cycle management.
• - Ensure compliance with regulations (e.g.,
HIPAA, ICD, CPT).
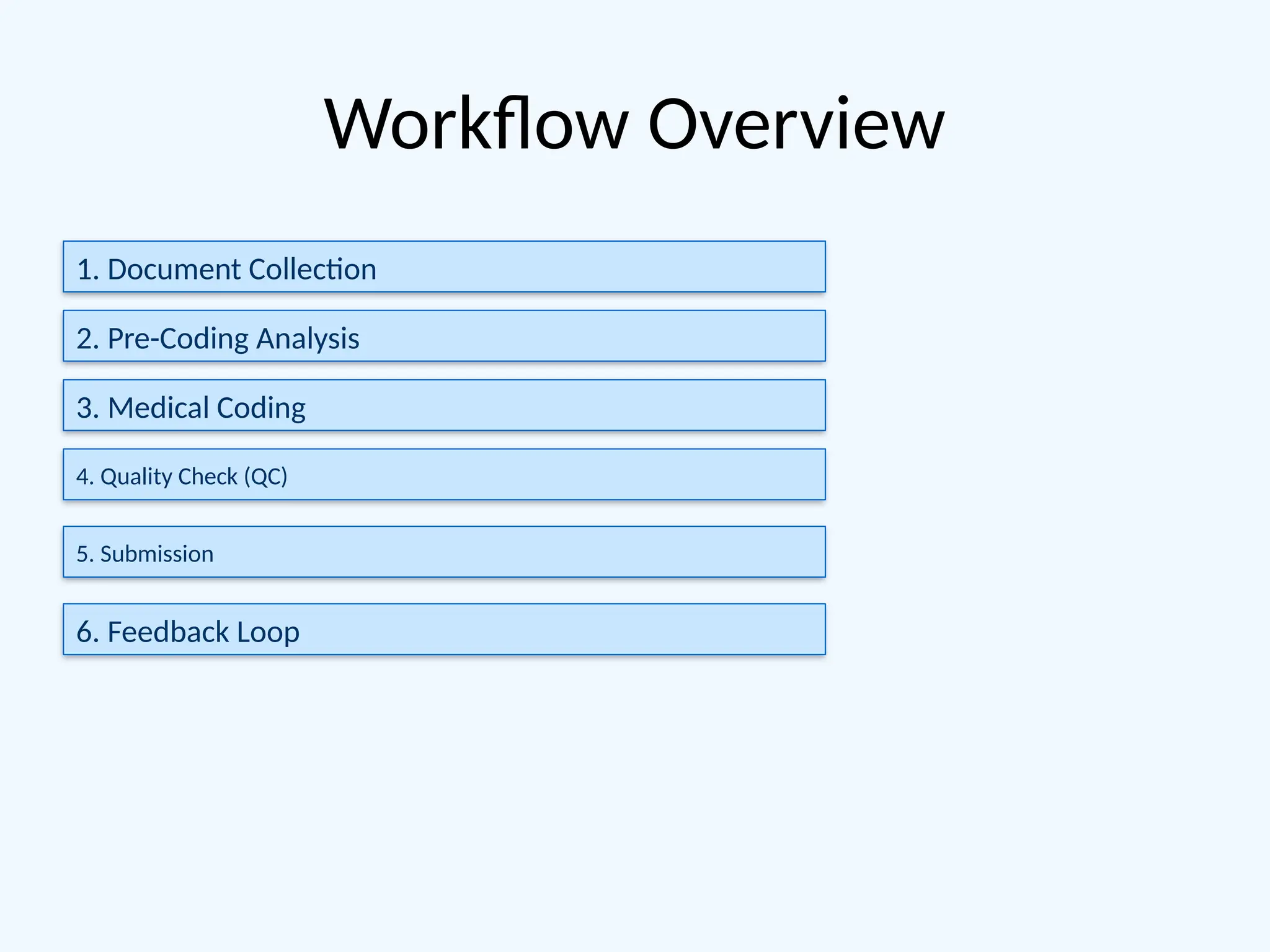
3. 4. Step 1 - Document Collection
• Details:
• - Sources: EMRs, physician notes, lab reports,
diagnostic imaging, etc.
• - Tools: Secure file transfer systems or cloud
platforms.
• Key Team Roles:
• - Data entry specialists, medical records
custodians.
5. Step 2 - Pre-Coding Analysis
• Details:
• - Verify completeness of records and eligibility.
• - Flag missing or ambiguous documentation.
• Key Team Roles:
• - Documentation specialists, compliance
officers.
6. Step 3 - Medical Coding
• Details:
• - Assign standardized codes (ICD, CPT, HCPCS).
• - Use coding software (e.g., Encoder Pro,
TruCode).
• - Ensure adherence to payer-specific
guidelines.
• Key Team Roles:
• - Certified coders (CPC, CCS).
7. Step 4 - Quality Check
• Details:
• - Audit codes against documentation for
accuracy.
• - Validate compliance with regulatory
standards.
• Key Team Roles:
• - Quality analysts, senior coders.
8. Step 5 - Submission
• Details:
• - Submit coded claims to billing or insurance
payers.
• - Track claim status and manage denials.
• Key Tools:
• - Revenue cycle management software.
• Key Team Roles:
9. Step 6 - Feedback Loop
• Details:
• - Review denials and corrections.
• - Implement process improvements.
• Key Team Roles:
• - Compliance officers, audit teams.
10. Tools and Technology
• Examples of tools:
• - EMR/EHR systems (e.g., Epic, Cerner).
• - Coding platforms (e.g., Optum360, 3M).
• - Quality audit software.
• Emphasize data security and HIPAA
compliance.
11. Team Roles and Responsibilities
• Overview of roles:
• - Medical coders.
• - Quality analysts.
• - Compliance officers.
• - Billing specialists.
• Training and certification requirements (e.g.,
AAPC, AHIMA).
12. Key Benefits of the Workflow
• Benefits:
• - Enhanced accuracy in claims processing.
• - Faster revenue cycle.
• - Improved compliance and audit readiness.
13. Conclusion
• Summary:
• - Efficient workflows ensure accuracy,
compliance, and client satisfaction.
• - Commitment to delivering high-quality
medical coding solutions.
• Contact details for further information.
Contact Us for More Information