Ruth Wetherald has over 30 years of experience as a registered nurse working in various areas including neurology, postpartum, labor and delivery. She recently earned a second bachelor's degree in healthcare information technology and is now pursuing a Master of Science in Nursing with a specialization in nursing informatics. Her goals are to obtain her master's degree and informatics certifications to qualify for a position in a non-profit organization working to improve healthcare technology and workflow.
































































![87
.Jalloh O, Waitman L. Improving Computerized Provider Order Entry (CPOE) usability by data
mining users' queries from access logs. AMIA ... Annual Symposium Proceedings / AMIA
Symposium. AMIA Symposium [serial online]. 2006;:379-383. Available from:
MEDLINE with Full Text, Ipswich, MA. Accessed April 24, 2016
Keough, V. A., & Tanabe, P. (2011). Survey research: An effective design for conducting
nursing research. Journal of Nursing Regulation, 1(4), 37–44.
Retrieved from the Walden Library databases.
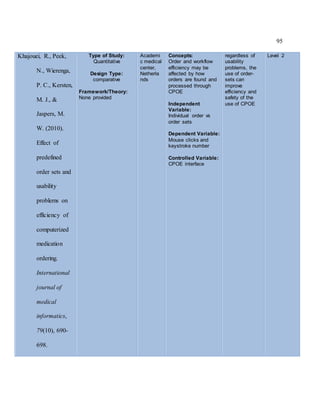
Khajouei, R., de Jongh, D., & Jaspers, M. W. (2009). Usability evaluation of a computerized
physician order entry for medication ordering. In MIE (pp. 532-536).
Khajouei, R., & Jaspers, M. W. M. (2010). The impact of CPOE medication systems' design
aspects on usability, workflow and medication orders. Methods of information in
medicine, 49(1), 3.
Khajouei, R., Peek, N., Wierenga, P. C., Kersten, M. J., & Jaspers, M. W. (2010). Effect of
predefined order sets and usability problems on efficiency of computerized medication
ordering. International journal of medical informatics, 79(10), 690-698.
Niazkhani, Z., Pirnejad, H., van der Sijs, H., & Aarts, J. (2011). Evaluating the medication
process in the context of CPOE use: the significance of working around the system.
International journal of medical informatics, 80(7), 490-506.
Peikari, H. R., Zakaria, M. S., Yasin, N. M., Shah, M. H., & Elhissi, A. (2013). Role of
computerized physician order entry usability in the reduction of prescribing errors.
Healthcare informatics research, 19(2), 93-101.](https://image.slidesharecdn.com/20326aaf-a451-44f3-bd62-73c5ae3ecd1c-160927013846/85/Wetherald-Master-s-CV-Resume-87-320.jpg)




![93
from access
logs. AMIA ...
Annual
Symposium
Proceedings /
AMIA
Symposium.
AMIA
Symposium
[serial online].
2006;:379-
383.
Available
from:
MEDLINE
with Full
Text, Ipswich,
MA.
Accessed
April 24,
2016](https://image.slidesharecdn.com/20326aaf-a451-44f3-bd62-73c5ae3ecd1c-160927013846/85/Wetherald-Master-s-CV-Resume-93-320.jpg)