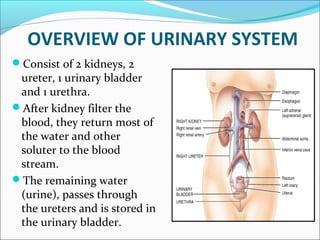
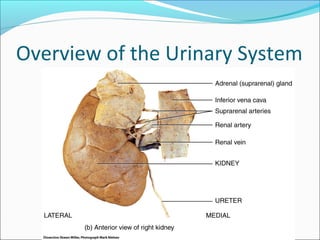
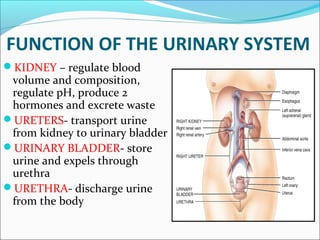
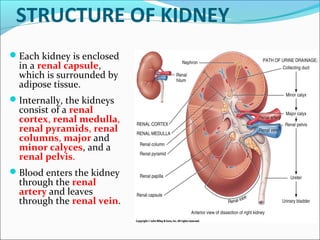
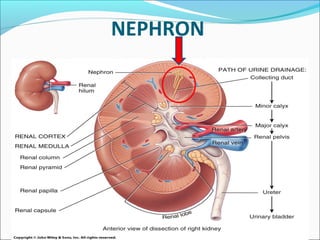
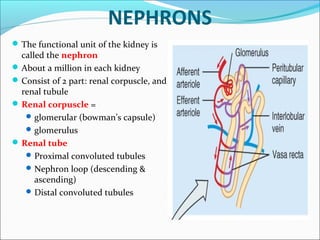
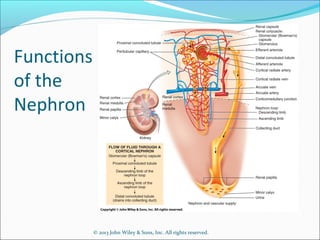
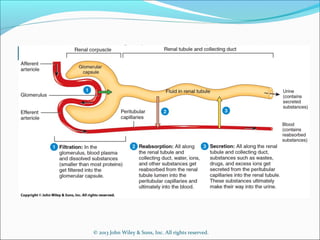
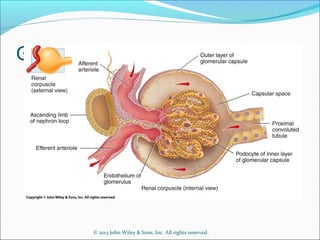
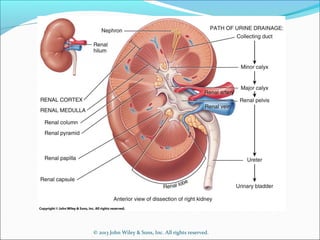
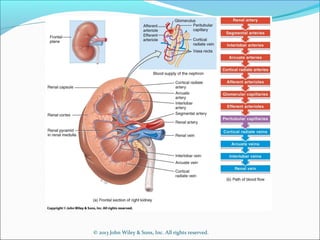
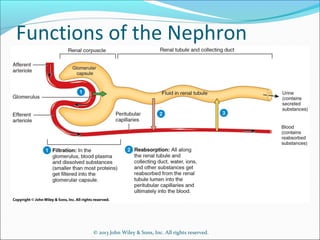
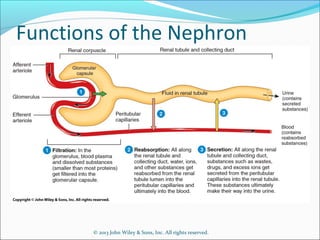
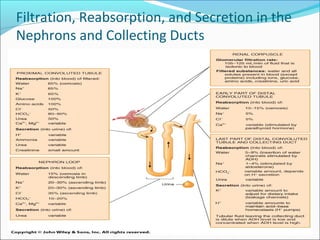
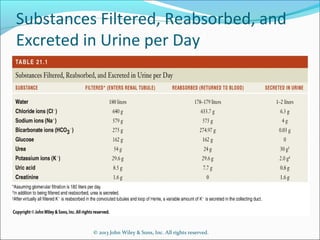
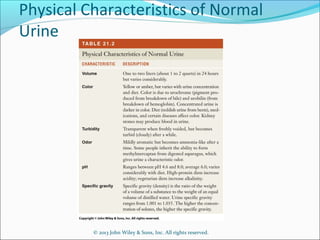
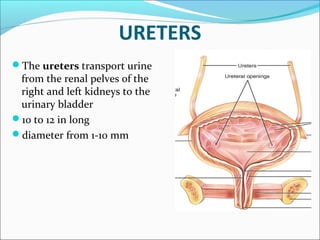
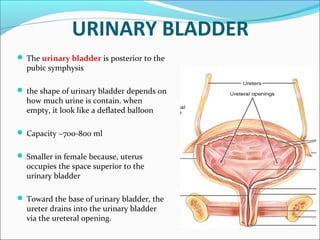
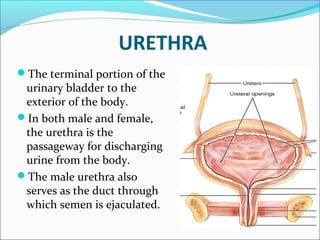
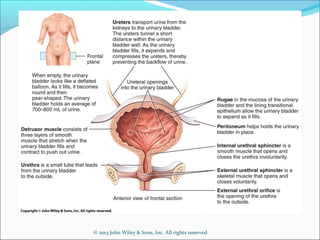
The urinary system consists of two kidneys, two ureters, one urinary bladder, and one urethra. The kidneys filter the blood and produce urine by regulating ions, volume, pH, and producing hormones. Urine passes from the kidneys to the bladder via the ureters. The bladder stores urine which is then expelled through the urethra. The functional unit of the kidney is the nephron, which filters blood and reabsorbs needed substances while secreting waste for urine production.