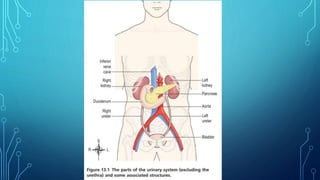
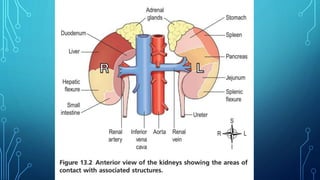
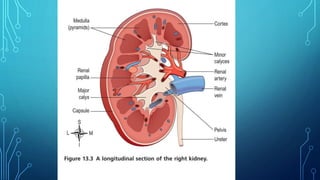
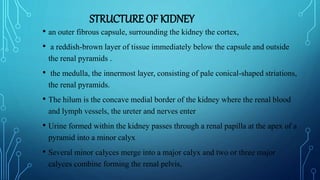
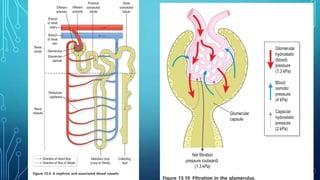
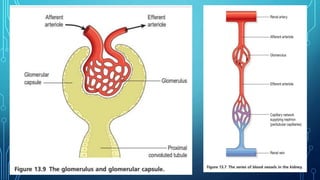
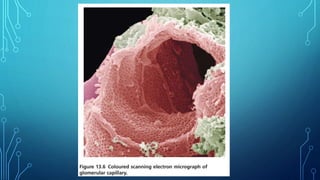
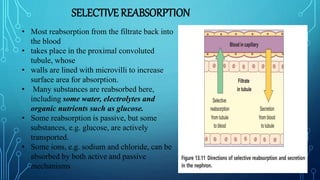
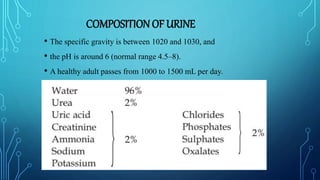
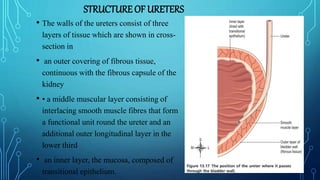
The document provides an overview of the human urinary system including its main components and functions. It discusses the anatomy and physiology of the kidneys, ureters, urinary bladder, and urethra. The kidneys filter waste from the blood to produce urine, which travels through the ureters to the bladder for storage. The bladder expels urine through the urethra under voluntary control. The document also describes urine composition and the processes of filtration, reabsorption, and secretion involved in urine formation in the nephrons of the kidneys.