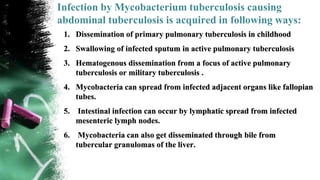
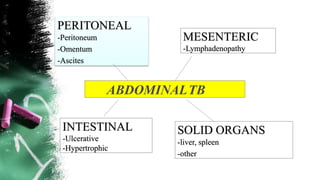
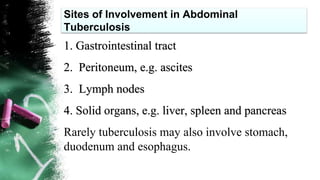
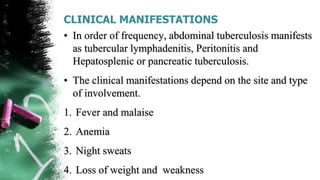
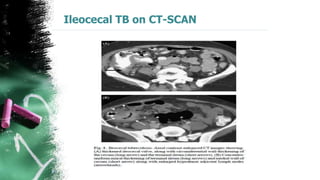
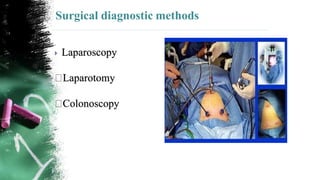
Abdominal tuberculosis is a common form of extrapulmonary tuberculosis that can affect the gastrointestinal tract, peritoneum, lymph nodes, and solid organs in the abdomen. It is caused by infection with Mycobacterium tuberculosis through ingestion of infected materials or hematogenous spread from other sites. Clinical manifestations vary depending on the involved sites but may include abdominal pain, diarrhea, fever, and weight loss. Diagnosis involves imaging tests like CT scans and laparoscopy along with biopsy and culture of affected tissues. Treatment consists of a standard 6-month antitubercular drug regimen, with monitoring for side effects like hepatotoxicity. Surgery is reserved for complications like perforation or obstruction.