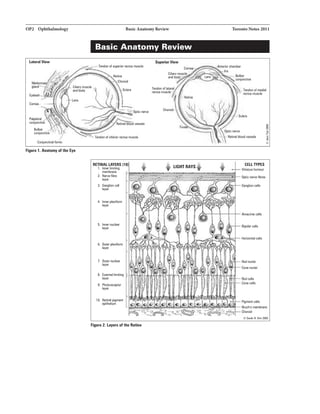
This document provides an overview of common ophthalmological topics including:
1) Basic anatomy of the eye, differential diagnoses for common presentations like vision loss and red eye, and ocular emergencies.
2) How to perform an ocular examination including assessing visual acuity, optics of the eye, and examination of structures like the orbit, lids, conjunctiva, cornea and more.
3) Common ocular conditions organized by structure or system affected such as the lacrimal apparatus, uvea, lens, vitreous, retina, glaucoma and others. Pediatric ophthalmology topics and ocular manifestations of systemic diseases are also reviewed.


![OP4 Ophthalmology Differential Diagnose5 ofCommon Presentations Toronto Notes2011
• anterior chamber
• uveitis (iritis, iridocyclitis)
• acute angle-closureglaucoma
• hyphema
• hypopyon
• endophthalmitis
T1ble 1. Common Differenti1l Di1gnosis of Red Eye
Conjunctivitis Acldllritis Ac.aAnale Keratitis
Cl01111 Glaucoma
Dildllrge Bacteria: purulent No No Profusetearing
Virus: 5erous
Allergy: mucous
Pain No ++ (tender globs) +++ ++(on blinking)
Plurtophobia No +++ + ++
Blurllld Vilian No ++ +++ Varies
Pupil Normal Smaller Fixed in rnid-(jilation Same ar smaller
ConjunctiVII with Ciliary Hush Dilluse Dilluse
liltal pallor
Com111 Normal aropacifiad KBratic precipitates StBIImy Infiltrate, adsma,
epithelial defects
Wraocular p...re Normal Varies lncraasad marlaKiy Normal ar increased
Anteriorchamber Normal Cells+ flare Shallow Cels + flare ornormal
Olher Large, lEnder Posteriorsynechiae Caloured haiDS
(auricLJar] node vil'lll NIIISea and vomiting
Ocular Pain
• differentiate from ocular ache: eye fatigue (asthenopia)
• herpes zoster prodrome
• trauma/foreign body
• keratitis
• corneal abrasion, corneal ulcer
• acute angle-closure glaucoma
• acute uveitis
• scleritis, episcleritis
• opticneuritis
• ocular migraine
Floaters
• vitreous syneresis (shrinkage and collapse ofvitreous gel)
• posterior vitreous detachment (PVD)
• vitreous hemorrhage
• retinal tear/detachment
• posterior uveitis
Flashes of Light (Photopsia)
• posterior vitreous detachment (PVD)
• retinal tear/detachment
• migraine with aura
Photophobia (Severe Light Sensitivity)
• corneal abrasion, corneal ulcer
• keratitis
• acute angle-closure glaucoma
• iritis
• meningitis, encephalitis
• migraine
Diplopia (Double Vision)
• binocular diplopia: strabismus, CNpalsy(Ill, IV. VI) secondaryto ischemia, diabetes,
tumour, trauma, myasthenia gravis, muscle restriction/entrapment, thyroid ophthalmopathy,
internuclear ophthalmologia (INO) 2°to multiple sclerosis, brainstem infarct
• monocular diplopia: refractive error, strands ofmucus intear film, keratoconus, cataracts,
dislocated lens, peripheral iridotomy](https://image.slidesharecdn.com/torontonotes2011ophthamology-230914210534-a58a727a/85/Toronto-Notes-2011-Ophthalmology-pdf-4-320.jpg)

![OP6 Ophthalmology
.....',
..
• OD oculusdut.r right wr-
• OS ocululi sinister lsft eyu
• OU =oculus uterqua =both eyes
.....' ,
..
A SnaUen viSUIIIacuity of2Qf2D aquabls
111 "normal" vision.
.....',
..
Infantand Child Villlll Acuity
• 6-12 months - 201120
• 1-2yell'$-2CV80
• 2-4 ye.,.. - 201'20
CFjCF
RIGHT m fields d111W1'1 on right side;
LEFT EYE fiulds drawn on lull side
{as ifseen through patient's eyes).
CF Able to count fingers in
spacified quadrant with
peripheral vision
Gross visual field deficit in
specified quadrant using
peripheral vision
Figure 6. Ophthalmology
Nomenclaturefor Visual Fialds by
Confrontation
.....',
..
For patients with dlllk iris11, IIISt the
pupils using an ophthalmoscopefocusad
onlha rad rellex. Thiswill provide a
b.u.rviM'than using a panlight.
....',
a.anglngliutiun from dilltance tu
_, r•• ilthe "near rwlllx"":
1. Eye convaroence
2. Pupil constriction
3. Lens accommodation
The Ocular Examination Toronto Notes 2011
• testing hierarchy for lowvision: Snellen acuity (20/x) -+ counting fingers at x distance (CF) -+
hand motion (HM) -+light perception with projection (LP with projection) -+ light perception
(LP) -+ no light perception (NLP)
• legal blindness is BCVA that is in the better eye, or a limit to the binocular central field
ofvision <20 degrees
• minimum visual requirements to operate a non-commercial automobile in Ontario are: with
both eyes open and examined together, 20/50 BCVA, a visual field of120 continuous degrees
along the horizontal meridian, and a visual field of15 continuous degrees above and below
fixation
Visual Acuity- Near
• use pocket vision chart (Rosenbaum Pocket VISion Screener)
• record Jaeger (]) or Point number and testing distance (usually 30 em) e.g. ]2 @ 30 em
• conversion to distance visual acuity possible (e.g. immobile patient, no distance chart available)
Visual Acuity for Infanta, Children, Non-English Speakers, and Dysphasics
• newborns
• visual acuity cannot be tested
• 3 mos-3 yrs (can only assess visual function, not acuity)
• test each eye fur fixation using an interesting object
• noted as "CSM• = central, steady and maintained
• 3 years until alphabet known
• pictures or letter cards/charts such as the HOTV or Sheridan-Gardner test (children point to
the optotypes on a provided matching card)
• tumbling "En chart
Colour Vision
• test with Ishihara pseudoisochromatic plates
• record number ofcorrectly identified plates presented to each eye, specify incorrect plates
• important for testing optic nerve function (e.g. optic neuritis, chloroquine use, thyroid
ophthalmopathy)
• note: red-green colour blindness is sexlinked and occurs in 7-10% ofmales
VISUAL FIELDS
• test "visualfields byconfrontation" (4 quadrants, each eye tested separatdy) for estimate of
visual field loss (Figure 6)
• accurate, quantifiable assessment with automated visual field testing (Humphrey or Goldmann)
or Tangent Screen
• use Amsler grid (each eye individually) to test for central or paracentral scotomas (island-like
gaps in the vision}, for patients with AMD
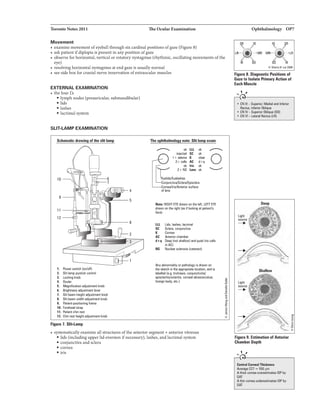
PUPILS
• use reduced room illumination with patient focusing on distant object to prevent "near reflex"
• examine pupils for shape, size, symmetry and reactivity to light (both direct and consensual
response)
• test for relative afferent pupillary defect (RAPD) with swinging flashlight test
• test pupillary constriction portion ofnear reflexby bringing object close to patient's nose
• "normal• pupil testing often noted as "PERLA" = pupils equal, round, and reactive to light and
accommodation
ANTERIOR CHAMBER DEPTH
• shine light tangentially from temporal side
• shallow anterior chamber: >2/3 ofnasal side ofiris in shadow (Figure 9}
EXTRAOCULAR MUSCLES
Alignment
• Hirschberg corneal reflex test
• examine in primaryposition ofgaze (e.g. straight ahead) with patient focusing on distant
object
• shine light into patient's eyes from -30 em away
• corneal light reflex should be symmetric and at the same position on each cornea
• strabismus testing as indicated (cover test, cover-uncover test, prism testing)
(see Strabismus, OP38)](https://image.slidesharecdn.com/torontonotes2011ophthamology-230914210534-a58a727a/85/Toronto-Notes-2011-Ophthalmology-pdf-6-320.jpg)

![Toronto Notes 2011 Optics
REFRACTIVE EYE SURGERY
• pennanentlyalters cornealrefractive properties by ablating tissue to changecurvature ofthe
cornea
• used for correction ofmyopia, hyperopia, and astigmatism
• common types includephotorefractivekeratectomy(PRK) and LASIK (see Surgical
ophthalmology, OP43)
• potential risks/side-effects: infection, undercorrection/overcorrection, decreased night vision,
cornealhau, dryeyes, regression, complete sever ofcorneal flap (LASIKonly)
Table Z. Optics
Pllllopllysialogy Clinical Flllu11s Trtllment Complications
Elmwtrupia • Image ofdisllrrt objects focus • Norefnlctiw em1r
Myopia
lfrperopil
exactly on 1he retina (Figure 12)
• Globetoo long relrtiw ID
refractive mechanisms, or
refractive mechanismstoo
strong
• "Nearsightedness" • Correctwi1h • Retinal tear/
• Usually presentsillst or nagative ciopter/ detachment,
2nd decede,atabilims in concava'"negative" macular hole,
2nd end 3rd decade; nnly lenses to diverge light openangle
• rays from distant object
focus in front ofretina -+ blurring
of(distance) vision (Figure 12)
begins after age 25 except in rays (Figure 13) glaucoma
patientswi1h diabiii8S • Refractive eyesurgery • Corrf)lications
orcalllracts not pr8V8111ed
• Blurring ofdislllnce wi1h refractive
vision; near viision usually correction
unaffected
• Prevalence of 30-40%in U.S.
populatim
• Globetoo short relative to
refractive mechanisms, or
refractive mechanismstoo
weak
• "Farsightedness" • When syrqJtomatic.
• You1h: usuallydo not require correctwi1h positive
glasses (still have sufficient Oiopter/COI1V8lll""plus"
accommodative abilityto lense& to COIIV8rge light
• rays from distant object
focus behild retina -+ blurring of
near ± distant vision (Figure12)
focus imageonretina), rays (Figure 13)
butmay develop • Refractive eyesurgery
• May be developmenllll ordue
ID any etiology 1hBIshoriBns
globe
accommodative esotropia
(see Stnlbismus, OP38)
• 30s-40s: blurring ofnear
vision due ID decreased
accommodation, may need
reading glasses
• >50s: blurring ofdislllnce
vision due ID severely
decreased accommodation
• rays not refracted uniformly • Affects approxinately30%
in all meridians due to of population, wi1h
non-spherical surface ofcom811S prevalence inCIIIIISing
or (e.g_ wi1hage
football-shaped) • Mild astigmatism
• Two types: unnoticeable
• Ragular- cuMIIuru • Hijler amount& of
uniformly differentin astigmatism may cause
meridians at rightanglesto blurry vision, s!JJinting,
each other as1henopia, orheadaches
• 1111111ular-distorllld cornea
causedby injury, karBioconus
(cone-shaped cornea),
corneal scar, orsevere
dryeye
• Normal aging process • Ifinitiallyemmetropic,
(>40 yeali) person beginstil hold
• Hardening/reduced reading material farther
of1he lens results in decreased away, but distancevision
accommodative ability remains unaffected
• Accommodative power is 140 at • Ifinitiallymyopic, person
age 10, diminishesto 3.50 by 40 removes distlrlce glasses to
• Near images cannotbe focused read
onto 1he retina (focus is behind • Ifinitiallyhyperopic,
1he retina as in hyperopia) ofpre5byapia
occur earlier
• Correctwi1h cylildrical
lens (ifregular),
trycontact lens (if
irregular)
• Refractive eyesurgery
• Correctwi1h positive
diopter/convex!"plus·
lenses for reading
• Angl&-closure
glaucoma,
particulal1y later
in life as lens
AliSDII'Ielropil • OiffwaJce in refractive em1rs
between eyes
• Second most
common cause
of amblyopia i1
children
Ophthalmology OP9
==@F
Emmetropil
==@F
Myopia
Hyperopia
Figura 12. Emmetropia and
Refractive Enors
]?@F
Hyperopia corrected wi1h
positive COIMIIlJiniJIBns
Myopia COIT8CI8d wi1h
negative divefvilg lens
Figura 13. Correction of Refractive
Errors](https://image.slidesharecdn.com/torontonotes2011ophthamology-230914210534-a58a727a/85/Toronto-Notes-2011-Ophthalmology-pdf-9-320.jpg)














![OP24 Ophthalmology
Treatmentfor aCllntral ratinal1118ry
occlusion !CRAOI must be initiated
within 2 hours of symptom onsatfor .,y
hope ofres!Dring vision.
llllldlVail Oa:luian Sludy IIIVDII
BllnchYain StudyGnllp:Argon lll8r
101macularedeml inbmui•'lein
accllsiaii.AmJOp/rlhllmD/19BUB: Zll-2112.
BVOSsiD.wd!hit arganilllrlrlltrr.ntim!1M1
sijlt inpetian1switiiiiiiCUaredan.
foiiiMing BRVO.Thetrublwrtalso._lha
riska1vmeoushem0111ge.
.....,,
,.}-----------------,
The "blood and thunder"" appeiii'BIIce on
fundoscopy is very characbristic of a
cenlrBI retinal vein occklsion {CRVOI.
Retina Toronto Notes 2011
Central Retinal Artery Occlusion (CRAO)- - - -
Etiology
• emboli from carotid arteries or heart (e.g. arrhythmia, endocarditis, valvular disease)
• thrombus
• temporal arteritis
Clinical Features
• sudden, painless (except in temporal arteritis), severe monocular loss ofvision
• relative afferent pupillary defect (RAPD)
• patient willoften have experienced transient episodes in the past (amaurosis fugax)
• fundoscopy
• "cherry-redspot" at centre ofmacula (visualization ofunaffected highly vascular choroid
through the thin fovea)
• retinal pallor
• narrowed arterioles, boxcarring (segmentation ofblood in arteries)
• cotton-wool spots (retinal infarcts)
• cholesterol emboli (Hollenhorst plaques) - usually located at arteriole bifurcations
• after -6 weeks: cherry-red spot recedes and optic disc pallor becomes evident
Treatment
• OCULAR EMERGENCY: attempt to restore blood flow within 2 hours
• the sooner the treatment =better prognosis (irreversible retinal damage if>90 min ofcomplete
CRAO)
• massage the globe (compress eye with heel ofhand for 10 s, release for 10 s, repeat for 5 min)
to dislodge embolus
• decrease intraocular pressure
• topical beta-blockers
• inhaled oxygen-carbon dioxide mixture
• IV Diamox- (carbonic anhydrase inhibitor)
• IV mannitol (draws fluid from eye)
• drain aqueous fluid- anterior chamber paracentesis (carries risk ofendophthahnitis)
• treat underlying cause to prevent CRAO in fellow eye
• follow up 1month to rule out neovascularization
Branch Retinal Artery Occlusion (BRAO)- - - - - - - - -
• onlypart ofthe retina becomes ischemic resulting in a visual fieldloss
• more likely to be ofembolic etiologythan CRAO; need to search for source
• management: ocular massage to dislodge embolus ifvisual acuity is affected
Central/Branch Retinal Vein Occlusion (CRVO/BRVO)
• second most frequent "vascular" retinal disorder after diabetic retinopathy
• usually a manifestation ofa systemic disease (e.g. hypertension, diabetes mellitus)
• thrombus occurs within the lumen ofthe blood vessel
Predisposing Factors
• arteriosclerotic vascular disease
• hypertension
• diabetes mellitus
• glaucoma
• hyperviscosity (e.g. polycythemia rubra vera, sickle-cell disease, lymphoma, leukemia)
• drugs [e.g. oral contraceptivepill (OCP), diuretics]
Clinical Features
• painless, monocular, gradual or sudden visual loss
• ±RAPD
• fundoscopy
• "blood and thundera appearance
• diffuse retinal hemorrhages, cotton-wool spots, venous engorgement, swollen optic disc,
macular edema
• two fairly distinct groups
• venous staaWnon-ischemic retinopathy
• no RAPD, VA approximately20/80
• mild hemorrhage, few cotton wool spots
• resolves spontaneously over weeks to months
• may regain normal vision ifmacula intact](https://image.slidesharecdn.com/torontonotes2011ophthamology-230914210534-a58a727a/85/Toronto-Notes-2011-Ophthalmology-pdf-24-320.jpg)




![Toronto Notes 2011 Glaucoma
• thinning, notching ofthe neuroretinal rim
• flame shaped disc hemorrhage
• 360• ofperipapillary atrophy
• nerve fibre layer defect
• large vessels become nasally displaced
• visual field loss
• slow, progressive, irreversible loss ofperipheralvision
• paracentral defects, arcuate scotoma and nasal step are characteristic
• late loss ofcentral vision ifuntreated
Treatment
• medical treatment: decrease lOP byincreasing the drainage and/or decreasing the production of
aqueous (see Glaucoma Medications, Table 10, OP45)
• increase aqueous outflow
• topical cholinergics
• topical prostaglandin analogues
• topical alpha-adrenergics
• decrease aqueous production
• topical beta-blockers
• topical and oral carbonic anhydrase inhibitor
• topical alpha-adrenergics
• laser trabeculoplasty, cyclophotocoagulation = selective destruction ofciliary body (for
refractory cases)
• trabeculectomy (see Surgical Ophthalmology, OP43)
• optic nerve head examination, lOP measurement and visual field testing to monitor course of
disease
• pachymetry to measure corneal thickness
Normal Pressure Glaucoma
• POAG with lOP in normal range
• often found in women >60 but may occur earlier
• damage to optic nerve may be due to vascular insufficiency
Treatment
• treat any causative underlying medical condition and lower the lOP further
Secondary Open Angle Glaucoma
• increased lOP secondary to ocular/systemic disorders that clog the trabecular meshwork
• steroid-induced glaucoma
• traumatic glaucoma
• pigmentary dispersion syndrome
• pseudoexfoliation syndrome
Primary Angle Closure Glaucoma
• 5% ofall glaucoma cases
• peripheral iris bows forward in an already suscept:J.ole eye with a shallow anterior chamber
obstructing aqueous access to the trabecular meshwork
• sudden shifting forward ofthe lens-iris diaphragm= pupillary block, results in inability ofthe
aqueous to flow from the posterior chamber to the anterior chamber and a sudden rise in lOP
(Figure20)
Risk Factors
• hyperopia: small eye, big lens -large lens crowds the angle
• age >70
• female
• family history
• more common in people ofAsian and Inuit descent
• mature cataracts
• shallow anterior chamber
• pupil dilation (topical and systemic anticholinergics, stress, darkness)
Ophthalmology OP29
bMiilnrllnnacdlr,_...-'GIIiuclml
l'llglllliln
120:1268-1279
S1udy: RlndalrDd COOO'ollldclinicll1rill.
l'llillb: 2.55 puticiiW, - ..clldllmlgh
I piiiUitianICII.pniiDI:Oi.llgld!iG-81with
rMydlllctJdopi!Hingil . .ilk!
dlllaell, •dandian irmaMirpn11110 001'1
d20IIIdta-
lillllrlllpicll IIIIHIIacka'!llltlmoQplaltgllll
lulrtllbeculaPniYarno inililllr8llmlal,with
- obsiMtionlorbothPIP'- Mldilli
-6ym.
...lkllaaml:!illtJCOI!IIpmgrusian• dllfinlld
byWulfieldIIIIIapti;dill: llbaarnJUtiel_
bnlll:l(f- Riducadby (1!1111115.1
T11ll'flg) illheIJealmenl Glu:on
prgareaion-Mlilrt in62rJindio.UJ• il11-.
The pruijntlllill-li(jllliclndv,.....
inlhahltmeot VI.11-. alllinlls.
Rule Ill' Furs
1/4 ol u-rlll population after u5ing
4weeks of topical steroid 4x/davwill
develop 111 increase in lOP.
lhlklllnlmlllilnalllrI'IIIIIIJa,..A191
Gllll:anlllldOc:U.......
C/rJrnDIII!JisetiS)'III!mlti:llellilws21101,
Issue 4.
lludr.Cocmn IMiwrJ Z611M
andme1Hnlf¥sis of10lrillsiMstilllliYJihe
dlupicllplllrlmcologi;III111111PM
far]Jii1wy111*11111111QiluCGII'IjPOAG) II OQIIIr
hyperlinsiun(0111)_
I'IIIMII: 4919 PlfliciparaIWidomiz8dii261Ji._
l'ltiera llldOIITwlbm-ulupressure(KI')
>21 IJidt.l orap1nqil(lllualml_
..........:1opi131 eye n.tlc:aliani, ilduding
blll-blackm.dormlllrida. brimulilila.
andepiletlllrilevenuseldioilier 1111 pllaillo.
llllil...-..: Re6JclionrJprogre..or
,.nond Glial afWulfilld dlllcts.
._..:MttHIII¥SiS on111111Uihll18118d
cWilsllllitstIDcahoarIIIINaiJd Clllllds
clernonslnlal11111bllerilgKf!educesinddence
d;uamllilllviullilkldlflciJ.withIll
oddsIIIia rJD-62 (M C1 0.47-0.811-llilwMr.
1MsRid is d mtadpractical 1118.me.
--.lillnpieswere pooled.No
dlmormiBd ignificllltwiullilkl pndlc:lion.
llawM!,n1 clnl,11111-blackmshawld
baldartnaliQMicenceinr8lb:ilg 1111111Ill
(lllualmlil patilllllwillDlfTwt.n Cll11fiiii(IID
pllcebo,Nih • OR of0.67!SClDA5-1.00).
c:.t111ianl: lawlringlOP Cllll'llb:lprogrlllian
ofllisuallil*ldefa:ls inpllierGwithOIIT.](https://image.slidesharecdn.com/torontonotes2011ophthamology-230914210534-a58a727a/85/Toronto-Notes-2011-Ophthalmology-pdf-29-320.jpg)

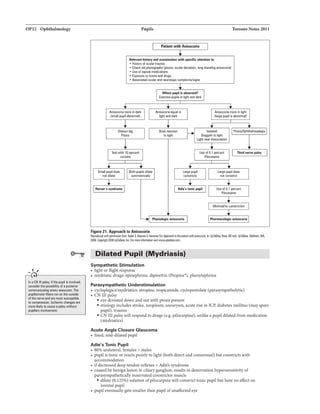
![Toronto Notes 2011 Pupils Ophthalmology OP31
Pupillary Light Reflex
• light shone directly into eye travels along optic nerve -+ optic tracts -+ both sides ofmidbrain
• impulses enterboth sides ofmidbrain via prc:tc:ctal area and Edinger-Westphal nuclei
• nerve impulses then travel down CN III bilaterallyto reach the ciliaryganglia, and finally to the
iris sphincter muscle, which results in direct and consensual light reflex
Pupil Abnormalities
Denervation Hypersensitivity
• when post-ganglionic fibres are damaged, the understimulated end-organ develops an excess of
receptor and becomes hypersensitive
• postganglionic parasympathetic lesions (ie. Adie's pupil)
• pupil will constrict with 0.12596 pilocarpine (cholinergic agonist), nonnal pupil willnot
• postganglionic sympathetic lesions (this test is used to differentiate between pre- and post-
ganglionic lesionsin Homer's syndrome)
• pupil will dilate with 0.12596 adrenaline, nonnal pupil will not
Local Disorders of Iris
• posterior synechiae (adhesions between iris andlens) due to iritis can present as an abnormally
shaped pupil
• ischemic damage [e.g. post-acute angle-closure glaucoma (ACG)]
• ischemic damage usually at 3 and 9 o'clock positions result in a vertically oval pupil that
reacts poorlyto light
• trauma (e.g. post intraocular surgery)
Anisocoria
• unequal pupil size
• idiopathic/physiologic anisocoria
• 2096 ofpopulation
• round, regular, <1 mm difference
• pupils reactive to light and accommodation
• responds normallyto mydiatrics/miotics
• see Table 6 for other causes ofanisocoria
Table 6. Summary of Conditions Causing Anisocoria
Futu1'81 Siteof!Mion Light ud Accommodation Anisocoria MwdrillictJMioticl EfftctofPilocarpine
ABNORMAL MIGnC PUPIL pmpairad pupiluy dilation)
Argyll-llobertsan Pupil negular, usuallybilateral
Ham•'• Syndrama Round. unilateral,
ptosis. amydrosis.
pseudoenophlhamos
Midbrain PoortD li;rt; bettErto
accommodation
Symplllheticsystem Bothbrisk
ABNORMAL MYDRIATIC PUPIL {impaired pupillaryconstriction)
Adie'a Tonic Pupil negular, la111er in bright light Ciliary Poorto betterto
accommodation
CN Ill Palsy Round CNIII ± fixed (acutely) at
7·9mm
Mwdrillic: Pupil Round, uni· arbilatural lri& !iphincllll' Fixsd at7·8 nm
Dilates/Constricts
Greaterin da!X Dilates/Constricts
Greaterin light Dilates/Constricts Constricts
(hypersensitivityto dilute
pilocarpins)
Greaterin light Dilate&IConstricts Constricts
Greaterin light No ulfsct Will not con&lrict](https://image.slidesharecdn.com/torontonotes2011ophthamology-230914210534-a58a727a/85/Toronto-Notes-2011-Ophthalmology-pdf-31-320.jpg)









![OP42 Ophthalmology
.....,,
Always test visual acuity (VA] first -
mlldicoi8QIII pratBction.
..... ,,
I!Rr if you•-any ofth-
llipl
• llec:relll8d VA
• ShaDow antlrior chamber
• Hyphema
• Abnonnal pupil
• Ocul11r misalignment
• Retinal damage
Manag11118111 of S.Piehld Glolle
Rapture
CAN'Tforget
Clorbib
Ancef IV
NPO
Tetanu..mtus
Shabn Bally Syndnlme
Syndrome of findings characterized
by no external signs ofabuse and
respimDry arrest, seizures, and
corTIII. Ocular axam findings 11r11
important for Shaken
Baby Syndrome. These findings
include amnsiv1 rwtinal and vitreous
hemorrhages 1hat occur during 1he
lhakilg proce11 and n extramely
rm in accidentll1nuna. Adetailed
fundoscopic exam or an ophthalmology
refemll should be conductEd for an
infants in whom abuse il suspected.
Pediatric Ophthalmology/OcularTrauma Toronto Notes 2011
Congenital Glaucoma
• due to inadequate development ofthe filtering mechanism ofthe anterior chamber angle
Clinical Features
• cloudy cornea, increased IOP
• photophobia. tearing
• buphthalmos (large "ox eye"), blepharospasm
Treatment
• filtration surgery is required soon after birth to prevent blindness
Ocular Trauma
Blunt Trauma
• caused byblunt object such as fist, squash ball
• history: injury, ocular history, drug allergy, tetanus status
• exam: VA first, pupil size and reaction, EOM (diplopia), external and slitlamp exam,
ophthalmoscopy
• ifVA normal or slightlyreduced, globe less likelyto be perforated
• ifVA reduced maybe perforated globe, corneal abrasion, lens dislocation, retinal tear
• bone fractures
• blowout fracture: restricted EOM, diplopia, enophthalmos (sunken eye)
• ethmoidfracture: subcutaneous emphysema oflid
• lids: swelling, laceration, emphysema
• conjunctiva: subconjunctival hemorrhage
• cornea: abrasion - detect with fluorescein staining and cobalt blue filter using slitlamp or
ophthalmoscope
• anterior chamber: assess depth, hyphema, hypopyon
• iris: prolapse, iritis
• lens: cataract, dislocation
• retinal tear/detachment
Penetrating Trauma
• include ruptured globe ± prolapsed iris, intraocularforeign body
• rule out intraocular foreign body, especiallyifhistoryof"metal striking orbit cr
• initialmanagement: refer immediately!!
•ABCs
• don't press on eyeball!
• don't checklOP ifpossibility ofglobe rupture
• checkvision, diplopia
• apply rigid eye shieldto minimize further trauma
• keep headelevated30-45° to keep IOP down
• keepNPO
• tetanus status
• give IV antibiotics
Hyphama
• bloodin anteriorchamber often due to damage to root ofthe iris
• may occur with blunttrauma
Treatment
• refer to ophthalmology
• shieldand bedrestx 5 days or as determined by ophthalmologist
• sleep with head upright
• may need surgical drainage ifhyphema persists orifre-bleed
Complications
• risk ofre-bleed highest on days 2-5, resultingin secondary glaucoma. corneal staining, and iris
necrosis
• never prescribe aspirin, as itincreases the risk ofare-bleed](https://image.slidesharecdn.com/torontonotes2011ophthamology-230914210534-a58a727a/85/Toronto-Notes-2011-Ophthalmology-pdf-42-320.jpg)


![Toronto Notes 2011 Common Medications Ophthalmology OP45
Mydriatics
• dilate pupils
• two classes
• cholinergic blocking (e.g. tropicamide [Mydriacyl•])
• dilation plus cycloplegia (lose accommodation) byparalysis ofiris sphincter and the
ciliary body
• indications: refraction, ophthalmoscopy, therapy for iritis
• adrenergic stimulating (e.g. phenylephrine HC12.5%)
• stimulate pupillarydilator muscles, no effect on accommodation
• usuallyused with tropicamide for additive effects
• side effects: hypertension, tachycardia, arrhythmias
Tabla 9. Mydriatic Cycloplegic Drugs and Duration uf Action
Dnlgs
Tropicamide (MydriacyP) 0.5%, 1%
Cydopentolate HCL 0.5%, 1%
Homatropine HBr1%, 2%
Atropine sulfate 0.5%, 1%
Scopolamine HBr 0.25%, 5%
Duman afAl:tian
4-5 hours
3-6 hours
3-7 days
1-2weeks
1-2weeks
GLAUCOMA MEDICATIONS
Tabla 10. Glaucoma Medications
Dnlg CAlgary
Alphi-AQonilt
No..lectin
o epilephrine HCI1%
o dipivalyl D.1% (Propine8
)
o brimonidine 0.2% (Aiphagan8 )
o apraclonidine 0.5%{Lopidine8 )
Beta-Blocker
No..lectin
o lirnolal (Timaptic•)
o lewbunolol{Betaganil})
Bm.-celective
o bstaxolol {Betoptic8 )
Carbonic AnhY*-Inhllilllr
o dorzolamide {Trusopt®)
o brinzolamide (Azopt®)
o oral: acetamlamide {Diamax®)
Pamymplthomimelic
{cholinergic stimulating)
o pilocarpine (Pilopine®l
o carbachol (l&apto
1gtt OSIOD bid/tid
1 gtt DSIOD qd,.tid
1gtt DSIODtid
Diamox8 : 500 mg
PO bid
1.Nort-&Bisctiw - "- production +
1'1M outflow
2. Selecliva- "- aqueous pralllction +
1' UY808clnl outflow
"- aqueous production
"- aqueous production
1-2 gtts DSIOD lill/qid 1'1M outflow
1. Non-selective - mydriasis, macular edema,tachycarcia
2. Selective-contactale111v. hypotension in chillhn
BrunchC11p81111 (cuelul in athiiii/COPD)
1' CHF
Bnulycardia
Hypotension
Depression
Heartblock
Impotence
••Mustaskaboutsulllllllergrl
Generally local side efh!cts with
topical preparlllions
Oral: diuresis, fatigue,
paresthesia&, Gl upset etc.
Miosis
-.1- ni;rtvision
1' Gl motiity
Brow ache
Headache
-.1-heartrate
Prasllgllndin Analog1111
o lillirlopra&t(Xalatan8 )
1gtt DSIOD qhs 1' uveoscleral outflow{uveoscleral responsible lri1 colour change
0 travaprast (JI'IIVllbll®)
for 20% of drainage) Periorbital skin pigmentation
Lash growth
o bimatoprost (Lumigan•)
timulol +doJZDimila; limciJI +h1Drlop!UII;Corrmig..• timobl+bri111111idine; lbl tinokll +1IMpust
WET AGE-RELATED MACULAR DEGENERATION MEDICATIONS
vascular Endothelial Growth Factors (VEGF) Inhibitors
Conjunctival hyperemia
• block vascular endothelial growth factor which prevents ocular angiogenesis and further
development ofchoroidal neovascularization
• administered via intravitreal injections
• pegaptanib (Macugen•) is a selective anti-VEGF targeting VEGF isoform 165
o ranibizumab (Lucentis•) is a non-selective anti-VEGF agent
o bevacizumab (Avastin•) is another non-selective anti-VEGF agent but is only FDA approved for
metastatic breast cancer, colorectal cancer and non-small cell lung cancer. Therefore, its use in
ophthalmologic is off-label](https://image.slidesharecdn.com/torontonotes2011ophthamology-230914210534-a58a727a/85/Toronto-Notes-2011-Ophthalmology-pdf-45-320.jpg)
![OP46 Ophthalmology Common Medications/References/Referen
TOPICAL OCULAR THERAPEUTIC DRUGS
NSAIDs
• usedfor less serious chronic inflammatoryconditions
Toronto Notes 2011
• e.g. ketorolac (Acular-), diclofenac (Voltaren•), nepafenac (Nevanac•) drops
Anti-Histamines
• used to relieve redanditchy eye. often in combination with decongestants
• sodium cromoglycate - stabilizes membranes
Decongestants
• weak adrenergic stimulating drugs (vasoconstrictor)
• e.g. naphazoline, phenylephrine (Isopto Frin•)
• rebound vasodilation with overuse; rarelycanprecipitate angle closure glaucoma
Antibiotics
• indications: bacterial conjunctivitis, keratitis, or blepharitis
• commonlyas topical drops or ointments, may give systemically
• e.g. sulfonamide (sodium sulfacetamide, sulfisoxazole),gentamicin (Garamycin•), erythromycin.
tetracycline,bacitracin, polymyxinB, fluoroquinolones (CiJ.oxan•, Ocuflmt"',VJg31Uax•, Zymar-)
Corticosteroids
• e.g. fluorometholone (FML•), betamethasone, dexamethasone (Maxidex•), prednisolone
(Predsol• 0.5%, Pred Forte• 1%), rimexolone (Vexol•)
• primary care ph)15icians should avoid prescribingtopical corticosteroids due to risk ofglaucoma,
cataracts, and reactivationofHSV keratitis
• complications
• potentiates herpes simplex keratitis and fungal keratitis as well as masks symptoms
• increased lOP, more rapidlyin steroid responders (within weeks)
• posterior subcapsular cataract (within months)
References
Complicztions: Your8Y'15&dilbftic retinopllhy. Clnldiln lilbel81Aaoc:iltion Nov2003.
lilbaticRatiiiiJFIIhy.Diabns Cara 1998;2111]:143·156.
liabet81 in OntJrio: 1111 IC6 l'rll:tica June 2003.
llloil
llrllord C. Illsic Oi*tfwlmolowforMedicalS1udlnand PrimuyCare R111id8111s. 7th ed.San Fnl11l:ilco:AmericanAcademyrJOphthalmology, 1199.
WIIDnFM.I'rlcti:alOphlllllmab.rl: AManuallor Begilninq llelidenbi. 41h ed. Americllll Academyrl Ophtlillmology,2005.
Frimlul N, Plned1R, KliArP. TheM11111ChulatllEyu1ndElr ManuIIrJ OphthalrnDIDII'f.Tmnlll:W.B. Saunders 1988.
KlnskiJJ.Clinical ASystamlticApproech. &1h lid.Oxhxd: llut18rwGrth·lllilem111ll, 2007.
S18in R,Stein H. Mnqernent Oc:ularEine'V'"Cill5. 41h ed.Mgntr111l: Medico11cept. 2006.
lllillilll
HuxJ.et al. Dlabll8sinOntario: an ICES l'nlc1iceAtlls.TGI'On!o: hstiMIforCiii:alEvluativa Sciences, 2003.
The CD!T1111itteefDIthe chmffiCitiDIIofretilopathyol premmrity.AnintemlliDnal cllssiliCitiDnolletinoPIIhYrJprar'llblrity.An:hOphlllai!DIDgy. 1984;102: 1130-34.
IIIIIIQII
Red Alln. www.radlllln.Grq
LII:Cini/Cia
llriYersi!y MicliiQIII KeiDgg EyeCentrewww.kltlgv.unicli.edWtheeyeslnrveMndu.html](https://image.slidesharecdn.com/torontonotes2011ophthamology-230914210534-a58a727a/85/Toronto-Notes-2011-Ophthalmology-pdf-46-320.jpg)