This document summarizes a study examining the relationship between post-traumatic stress disorder (PTSD) and suicide among US service members and veterans of the Iraq and Afghanistan wars. It notes that 11-20% of military members from those wars have been diagnosed with PTSD, and about 22 service members die by suicide per day, surpassing combat deaths. The study reviews past research on PTSD and interviews veterans diagnosed with PTSD. It aims to provide insight into factors contributing to the link between PTSD and suicide.

![3
Introduction- Approximately 1.7 million United States’ Troops have been deployed since the
start of the Afghanistan and Iraq wars and of those Troops, approximately one third came from
our part time Military (National Guard & Reserve Units)[3]. Many of these Troops from the
United States will do more than one deployment to a combat zone in at least one of these
countries. With a RAND (a private non-government organization that studies the many effects of
the military members) study done in 2008 it was estimated that 300,000 United States Troops
met the criteria for posttraumatic stress disorder or depression which is about 18.5 percent of the
total troops deployed at that time [3]. This number may seem low in the bigger picture of the
amount of total Troops deployed, but if you take to in account that most of these Troops will
come home to some type of family or loved ones, this stress disorder can have a heavy effect on
those around the Service Members. Starting in April 2003 the Department of Defense started
requiring deployed Service Members to take a post deployment health assessment upon their
return. With the war in Afghanistan starting in 20001 there was a three year period where
deployed Service Members had no such assessment; they had no type of assessment and were
left to figure it out on their own. The idea of a post assessment was a start in figuring out how the
Department of Defense could help its returning Service Members, but what they didn’t take in to
account, was most of the posttraumatic symptoms didn’t come forward until later on down the
road once the Service Members were home for about three months. In response the Department
of Defense initiated a second assessment called (PDHRA) which was a reassessment about three
months after the first initial assessment. Once again many Service Members have fallen through
the cracks of the system [5]. Service Members dealing with the undiagnosed or diagnosed
symptoms with posttraumatic stress disorder are very unique and distinctive. Service members
with PTSD can go through a variety of issues such as, flashbacks, trouble sleeping or not](https://image.slidesharecdn.com/1ba0db0e-d42c-4c9e-a9df-a7131e044936-160429203352/85/Thesis-Paper-3-320.jpg)

![5
Literature Review: I will be reviewing the article “Mental Health Care for Iraq and Afghanistan
War Veterans." By Burnam, M. A., L. S. Meredith, T. Tanielian, and L. H. Jaycox. The mental
health of our returning Troops from the wars in Afghanistan and Iraq is a huge challenge because
of the unforeseen consequences of the dark side of war and its effects on the human physique. In
any war there is always trauma and cases of mental obstacles to overcome. The issues that have
come to the forefront besides the inadequate service of the Veterans Affairs is that there are
many Services Members that are not coming forward to receive help with their issues. Service
Members not coming in for treatment and assessments is not necessarily because they are
reluctant to do so but because they may not trust the system to take care of them. The Service
Members also have a silent code to suck up any and all injuries and drive on with the mission
without stopping.
There are many steps that need to be taken to elicit the proper care for the Troops
returning from combat. One of the steps involves our part time troops in the National Guard and
Reserve Units across the United State. The National Guard and Reservists upon returning from
their deployment can pay for continued health insurance with TRICARE. TRICARE is
affordable but it still comes at the cost of the Service Member to continue to receive benefits to
get help. About 74 percent of the activated part time Service Members return to their civilian
jobs and about 20 percent retire from the service. In either situation the Service Member has to
pay out of pocket [3]. This is just one example the author gives where it makes it harder for the
service member to get help. Making the Service Member pay for help after he or she serves her
country is an insult; then their benefits are reduced or limited. Although the Service Member
loses his or her benefits, if they may qualify for further benefits with an injury sustained from
combat or their services. The Services Member may receive up to 5 years of extended benefits to](https://image.slidesharecdn.com/1ba0db0e-d42c-4c9e-a9df-a7131e044936-160429203352/85/Thesis-Paper-5-320.jpg)
![6
correct that particular ailment. The only problem with getting that extra 5 years is that the burden
falls on the Service Member to prove it was service connected. The Service Member will have to
jump through hoops and endure an agonizing process to retain the benefits.
This article demonstrates that there is a serious disconnect and a baseline standard when
it comes to diagnosing and dealing with returning Service Members from combat in the Iraq and
Afghanistan wars. The authors describe the system in which diagnoses and treatments have an
unequal standard in placement of facilities to take care of our Service Members. On page four of
their article they state that most specialists concentrate on the urban areas and less on the rural
areas of the United States leaving many Service Members without adequate treatment [3]. Those
living in the rural areas now have the burden to travel to get the help they need. Some of these
Service Members will have to drive hours, in some cases, to receive their treatment leaving them
demoralized and discouraged. The constant traveling becomes grueling and takes a toll on the
Service Member, ultimately, it’s not worth it given the time and money spent to meet the
appointment. The other burden is if a Service Member misses any appointments they become
non-compliant and can be disqualified from their benefits. These strains on the Service Member
with an already melting pot of issues that they are combating makes the drive not worth it. Once
again the Service Member can only rely on themselves and have to go it alone and “suck it up”.
The Service Member is once again left on their own to combat their issues, which can have them
travel that slope of anguish. The Service Member may think they have no other option to stop the
pain that they are dealing with and the pain they cause others.
The authors Burnam, M. A., L. S. Meredith, T. Tanielian, and L. H. Jaycox stated in their
research "Military culture promotes pride in inner strength, self-reliance, toughness, and being
able to “shake it off” ailments or injuries.”[3] When a Service Member arrives to their](https://image.slidesharecdn.com/1ba0db0e-d42c-4c9e-a9df-a7131e044936-160429203352/85/Thesis-Paper-6-320.jpg)
![7
perspective basic training site when they enlist in to the military they go through many weeks of
extreme stress of physical and psychological pain. You are broken down and rebuilt from the
ground up; it is meant to push your body to its breaking point without breaking. This is supposed
to make you tough internally as well as externally. The whole idea of “suck it up” comes from
this very process. When you spend enough time sucking it up and driving on without coming
forward it has a tendency to stick with you long after your service is over [7]. With the head
strong mentality that was instilled in the Service Member from the start of their careers and the
unsaid code of “suck it up”, it can also be a hindrance of seeking help when a serious enough
issue arises such as posttraumatic stress disorder. It is completely clear that because of this, the
Service Members try to tough it out and go it alone. With posttraumatic stress disorder, going it
alone, and toughing it out mentality does not mix well for the survival of the Service Member.
Combating posttraumatic stress disorder without the proper tools and help is like sending a
Soldier to war without guns and the preparation to survive in combat. The Service Members
reluctance to seek help because of the chance of embarrassment of being seen as weak could
have them so deep and dark in to a hole and pushed up against a wall, it may lead to only way
out and that is suicide. Suicide becomes the means to the end of suffering and quitting the
constant struggle of combat back home.
This article gave a great insight on the services that are provided and the great deal of
work that the Service Members have to go through to get the proper care and assessments that
they need to get better. The authors do in my opinion a remarkable job showing the stresses and
the less than adequate facilities in certain areas. With a Service Member already combating their
posttraumatic stress disorder and now the added stress to fight harder because the burden has
been put on them instead of being taken care of when they return home from war, may cause a](https://image.slidesharecdn.com/1ba0db0e-d42c-4c9e-a9df-a7131e044936-160429203352/85/Thesis-Paper-7-320.jpg)
![8
point of breaking and then surrender to the battle. It is my opinion that this article has put forth
evidence in the connection between posttraumatic stress disorder and the added pressure that the
Service Member has to go through to survive in what may seem as an unappreciative
government that has left them in the wind.
The second research article I will be reviewing is Abigail C. Angkaw, Giao Q. Tran,
David A. F. Haaga. “Effects of training intensity on observers' ratings of anxiety, social skills,
and alcohol-specific coping skills” [1]. In this article the authors research the differences in how
clinicians rate a Veteran with posttraumatic stress disorder, anxiety, alcohol usage, coping skills,
and bias of the rater. When a Veteran goes to the Veterans Affairs to seek help they will meet
with a psychologist to be examined for any mental disorder. This is a crucial meeting to
determine what type of mental disorder the Veteran is suffering from, so they can adequately
treat them for any mental disorder. The Doctors use a rating scale as a tool in the assessment to
characterize the observed disorders, so they can properly diagnose a treatment. The rating
portion of the Doctor is vital to the assessment, which will depict the psychometric
characteristics of the veterans’ disorder.
The Authors found this process as a point in their research to determine if our veterans
were getting a proper ratings. This would in turn give them the adequate treatment they needed
to get better. Because the rating is vital to their treatment, it must be reliable to determine what
the course of action will be taken to treat the Veteran. The Authors examined the many types of
trainings and styles that the Doctors will undertake before they can rate a Veteran. Some of the
trainings are; rater error training and frame-of-reference, which are used to lower the error of
ratings. The Authors discovered that the Doctors will undergo some training but not what they](https://image.slidesharecdn.com/1ba0db0e-d42c-4c9e-a9df-a7131e044936-160429203352/85/Thesis-Paper-8-320.jpg)


![11
were not offered any type of compensation or promises. The research subjects were all
volunteers and contributed the information at their own free will. The research subjects were at
the start of the interviews were only offered sources and outlets to help them with any
reoccurring traumas that may come up during the research process.
Data: Table 1. This study that was conducted by Stevens, Daniel and his colleagues [10] with
1,433 participants. The research compares the characteristics of trauma leading to posttraumatic
stress disorder in association to suicide. This shows the lifetime attempts and the traumatic
exposures across subgroups depicting the relationship between posttraumatic stress disorder and
suicide. The mean age of the participants was 39 at the time the interview was conducted. The
table also shows that out of all the participants, 402 of them have had an indication of prior
attempted suicide which is about (28%). In the study the table also shows that the majority of the
participants had, in fact, experienced at least one traumatic or life threatening event and about
14% had been diagnosed with posttraumatic stress disorder. It was clear that that woman had a
more likely chance of experiencing trauma and that there were was no big significant difference
in the educational levels. The one thing that did stand out in this table and the research is it
depicted that minorities were more likely to obtain posttraumatic stress disorder over others.](https://image.slidesharecdn.com/1ba0db0e-d42c-4c9e-a9df-a7131e044936-160429203352/85/Thesis-Paper-11-320.jpg)
![12
TABLE 1.
In another study done by Veterans and PTSD [11] with the RAND study found that out of
the 2.7 million Service members that served in Iraq and Afghanistan (20%) of them have
posttraumatic stress disorder. Most of the clinicians state that they believe that number is even
Characteristics
Noattempt
(n=179)
Attempt
(n=33)
Noattempt
(n=735)
Attempt
(n=281)
Noattempt
(n=117)
Attempt
(n=88)
Gender
Female 138(83) 27(17) 615(73) 229(27) 102(68) 75(42)
Male 41(87) 6(13) 120(70) 52(30) 15(54) 13(46)
Race
Minority 19(90) 2(10) 46(60) 28(40) 17(50) 14(50)
Non-Minority 160(80) 31(20) 689(73) 253(27) 100(57) 74(43)
Age
19-29 79(90) 9(10) 220(73) 84(27) 27(57) 20(43)
30-39 47(86) 7(14) 210(75) 72(25) 72(25) 25(54)
40-49 24(75) 8(25) 140(69) 64(31) 38(61) 24(39)
>50 29(76) 9(24) 165(73) 61(27) 31(62) 19(38)
Education
H.S.orless 18(82) 4(18) 61(67) 32(33) 8(47) 9(53)
College 96(86) 15(14) 360(68) 171(32) 66(58) 48(42)
Adv.Studies 65(82) 14(18) 314(80) 78(20) 42(58) 31(42)
*Abbreviation:PTSD,PosttraumaticStressDisorder
NoTraumaExposure
(n=212; 15%)
TraumaExposurewithout
PTSD(n=1016;71%) PTSD(n=205;14%)
n(%)
TABLE1.Lifetimesuicideattemptandtraumaticexposureacrosssubgroupsofthesamplepopulation](https://image.slidesharecdn.com/1ba0db0e-d42c-4c9e-a9df-a7131e044936-160429203352/85/Thesis-Paper-12-320.jpg)
![13
higher with all the unreported or mild cases. The report also states that the number of reported
posttraumatic stress disorder case is increasingly higher than any other conflict. In this study it is
reported that suicide rates are much higher than was initially thought with an average of 22
military/Veterans related suicides a day, that is about 5-8 thousand reported cases a year among
the ranks in the military/Veterans. The distribution of posttraumatic stress disorder throughout
the military are: Army (67%) of cases, Air force (9%), Navy (11%), Marines (13%), which can
be found in the (Congressional Research Service) [11]. Another study done by "Mental and
Physical Health Status and Alcohol and Drug Use Following Return from Deployment to Iraq or
Afghanistan." Susan V. Eisen, PhD, in a research study that was done with 600 Service Members
with posttraumatic stress disorder showed a substantive amount of alcohol abuse. The percent of
Service Members that reported that they have a problem with abusing alcohol was 39% and drug
use was 3%. Also within that study it was reported that major depression was an issue. In a
recent study of 460,000 Veterans of the Afghanistan and Iraq war [13] reported a significant
increase in suicide among Veterans with a posttraumatic stress disorder with a mortality rate of
1.33 and those who were under the care of the Veterans Affairs were 1.77 which is a slight
increase because of the troop serge and the amount of increased traumas from war.](https://image.slidesharecdn.com/1ba0db0e-d42c-4c9e-a9df-a7131e044936-160429203352/85/Thesis-Paper-13-320.jpg)
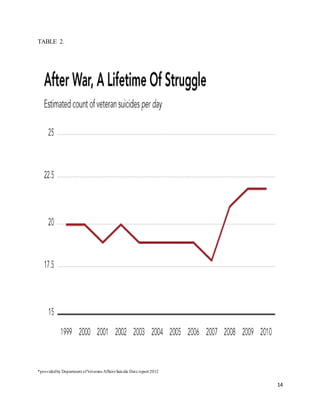
![15
This table was taken from a report done By the Department of Veterans Affairs [12]
showing the alarming rate of suicides among Veterans. The Graph shows that between the start
of the war in Afghanistan in 2001 with a minor spike in 2002 pretty much remained steady until
2008 when the major surges happened in Iraq. From 2008 and on the rise of suicides among
Veterans rose at an alarming rate. The graph also shows that suicide amongst Veterans after their
services has been completed has a major toll on a person’s psyche. Although this is only an
estimate it is clear that in the height of the two wars in Iraq and Afghanistan the rate of suicide
rose and the amount of diagnoses of posttraumatic stress order also increased. There was also a
minor dip in the suicide rate in 2007. This could be explained due to the amount of troops
deployed to the combat zones and very few were left here in the United States to dwell on their
traumas and stresses. While in combat the service members are numb to emotions and stress
because they are not sitting around to feel and think about all that they have scene. It didn’t go
back up until the troops in 2008 started to return from their rotations from the initial surge.](https://image.slidesharecdn.com/1ba0db0e-d42c-4c9e-a9df-a7131e044936-160429203352/85/Thesis-Paper-15-320.jpg)
![16
TABLE 3.
Table 3. Is a graph provided by the Department of Veterans Affairs From 2002 to 2008, it
shows suicides per 100,000 Veterans who were enrolled in the VA Health Care. [12]. The data
shows that there is a major gap between female Veterans and male Veterans. The reason that
there is a gap between male and female Veterans is because of the roles that each sexes plays in
the war efforts. Traditionally women were not allowed on the front lines of the fighting, women](https://image.slidesharecdn.com/1ba0db0e-d42c-4c9e-a9df-a7131e044936-160429203352/85/Thesis-Paper-16-320.jpg)
![17
were assigned in a more supportive roll, such as Military Police, Engineers, Administration, and
other rolls. To be fair to their services and not discredit them and their roll which were crucial to
the success of the mission, they experienced trauma as well. As the wars dragged on we
witnessed more and more females fighting on the front lines, but this wasn’t prevalent until later
in the war. The most alarming part is all these Service Members were in the care of the Veterans
Affairs seeking help. This is truly alarming.
There are many Service Members that are left in the wind when they come back from
their perspective tours in Iraq and Afghanistan. The Veterans that carry the weight of
posttraumatic stress disorder from serious combat incidences after serving in Iraq or
Afghanistan. In the RAND study only about half of those who tested positive and met the criteria
for posttraumatic stress disorder or depression received or sought care in their mental health
disorder from the inflicted traumas in the wars in Iraq and Afghanistan. Then less than half of
those who received the treatment got adequate or proper help from their perspective clinics or
treatment centers. In the RAND study those with mental health problems with no treatment were
8.8%, those with no mental health problems were 81.5%, those with mental health problems with
any treatment were 4.1%, and those with mental health problems had minimally adequate
treatment were 5.6%. The facilities in lower priority statuses are most likely to deter the Veteran
because of the inadequate services and treatment that they provide. Getting some treatment is
better than none, but because the Veteran has to deal with their own issues the last thing they
want to deal with is the stress from inadequate treatment. Because of the inadequate services the
stress of the Veterans increases and can only compound the issue of not seeking help [3].
Emotional hiding of is a constant struggle that is hard to cope with. In a study that was
done by Daux, Jeanne in a sample of 400 Veterans with posttraumatic stress disorder, they were](https://image.slidesharecdn.com/1ba0db0e-d42c-4c9e-a9df-a7131e044936-160429203352/85/Thesis-Paper-17-320.jpg)
![18
less likely to share their emotions about their traumatic events. The study also determined that
the less the Veteran ignores and hides their emotions from social support groups and people the
more likely their posttraumatic stress disorder will get worse and overcome them. The study
showed that disclosing a traumatic event is more likely to help heal the wounds of combat and
their posttraumatic stress disorder. The research also concluded that combat exposure and the
stress of deployments increases the chance of posttraumatic stress disorder, depression,
substance abuse, and impairments in functioning in society. The withdrawal from social
encounters and support are directly symptoms from posttraumatic stress disorder [4].
In a study done by Hannold, Elizabeth depicting the issues with Veterans and driving
after their combat deployments. In the authors research it shows that after a Veteran returns
home after a deployment there chances of vehicular accidents rises by 13%. The study also
shows that Veterans returning have issues adjusting back home when it comes to driving because
of the tactical mind set of combat driving. Some of the terms that describe Veterans and driving
are aggressive, rage, hyper alert, and disregard for others. Driving triggers that make the Veteran
anxious are big trucks, crowds, highway traffic, driving small vehicles, loud or distracting noises,
driving in the dark, getting lost, and being in the rain. The research also determined that stress
and anxiety in Veterans hinders and impairs their driving which speaks to the increased vehicle
accidents upon returning from combat [5].
I conducted a study involving 5 independent Veterans answering a serious of questions in
their experience with posttraumatic stress disorder in conjunction with suicide. The series of
questions are asked with an open-ended answer for the Veteran. There are five questions: 1. Do
you suffer from posttraumatic stress disorder? 2. Are you currently receiving care from the
Veterans Affairs or the VHA? 3. Have you ever thought about or acted on the idea of suicide?](https://image.slidesharecdn.com/1ba0db0e-d42c-4c9e-a9df-a7131e044936-160429203352/85/Thesis-Paper-18-320.jpg)

![20
disorder is so bad that they have to take a candy store of drugs that are prescribed to them and all
the drugs that they have to take leaves them laying on their couch like a vegetable. The Veteran
also is fearful in the amount of prescribed drugs they have to take. This Veteran also stated that
he was told by his health care providers that if he didn’t take the prescribed drugs he could be
found non-compliant and could lose all his benefits. The last comment that was made about the
services that they were trying to receive from the Veterans Affairs was that they were treated as
if they were just another name on a piece of paper and were not treated like a person or human
being.
Analysis: This research is to determine the connection between posttraumatic stress
disorder and suicide. I will be analyzing the data used for this research to prove my hypothesis
that there is a connection. It is hard to fathom that our Veterans go to war in many cases multiple
deployments only to be discarded when their services were rendered. The connection between
posttraumatic stress disorder and suicide may not have a direct line to one another, but it is clear
that there are issues that contribute to suicide in conjunction with posttraumatic stress disorder.
It is clear that no matter who you are or where you are from posttraumatic stress disorder can
affect anyone. It doesn’t matter your education level or where you are from the only thing that
matters is that a traumatic event can haunt the mind and psyche of our Veterans. In Stevens,
Daniel’s research he shows that those dealing with posttraumatic stress disorder have a more
likely chance of committing suicide than a normal person without any major traumatic
incident[10]. Posttraumatic stress disorder is a struggle with the will of the mind to overcome an
event so traumatic that in itself could be life or death. This was prevalent in Stevens, Denial’s
research where he discovered that in his research of 1,433 participants with posttraumatic stress
disorder, 402 (28%) of them had signs of attempting suicide more than once. This is evidence](https://image.slidesharecdn.com/1ba0db0e-d42c-4c9e-a9df-a7131e044936-160429203352/85/Thesis-Paper-20-320.jpg)


![23
The RAND study told us that of those who met the criteria and tested positive for
posttraumatic stress disorder or depression only half of them sought help from the Veterans
Affairs. Of those who sought help half of them received inadequate treatment for their traumas of
war. The RAND study produced an extreme issue of coverage for those who have met the
criteria for posttraumatic stress disorder. The second highest stat in conjunction with the study on
mental health problems was Veterans that tested positive didn’t receive assistance with their
posttraumatic stress disorder. The third highest stat was that those who met the criteria received
help and it was minimal and less then acceptable services.
Veterans coming back from combat have a tendency to withdraw and hide their emotions
when talking about their experiences form their deployment. Veterans with posttraumatic stress
disorder are more likely not able to associate with society. Veterans feel as if people don’t
understand them and don’t know what they are going through because of their traumatic event
experienced in combat. Other issues such as alcohol, and drugs are disabling products of the
need not to feel and forget. This makes it harder to gain any sort of control to seek help. All these
vices do is disable the Veteran to a point of hopelessness. Seeking help through the Veterans
Affairs or some type of community outreach program can help in the recovery of posttraumatic
stress disorder and lift the heavy weight they carry. Veterans are reluctant to trust anyone outside
of their units and friends in the military because of the bond they build on deployment. Trust is a
priceless value that Veterans don’t give out and because of that it makes it harder for them to
seek help and share their story with others.
Aggression and driving is just one major issue because Veterans are 13% [5] more likely
to get in an accident when returning home from war. Veterans have a hard time assimilating back
to society and what is real and what is just in their head from war. There are many stories of](https://image.slidesharecdn.com/1ba0db0e-d42c-4c9e-a9df-a7131e044936-160429203352/85/Thesis-Paper-23-320.jpg)






![30
9. Shiner, B, et al. "Access To VA Services For Returning Veterans With PTSD." Military
Medicine 177.7 (2012): 814-822.
10. Stevens, Daniel, et al. "Posttraumatic Stress Disorder Increases Risk For Suicide Attempt
In Adults With Recurrent Major Depression." Depression & Anxiety (1091-4269) 30.10
(2013): 940-946. Academic Search Premier. Web. 4 Mar. 2015.
11. http://www.orlandosentinel.com/news/opinion/os-ed-veterans-affairs-health-care-
080813-20130807,0,666522.story
12. http://www.va.gov/opa/docs/suicide-data-report-2012-final.pdf
13. “Veterans statistics: PTSD, Depression, TBI, Suicide.” Veterans and PTSD. February 14,
2015. Web. [month, day, year accessed.] www.veteransandptsd.com/PTSD-statistics.html](https://image.slidesharecdn.com/1ba0db0e-d42c-4c9e-a9df-a7131e044936-160429203352/85/Thesis-Paper-30-320.jpg)