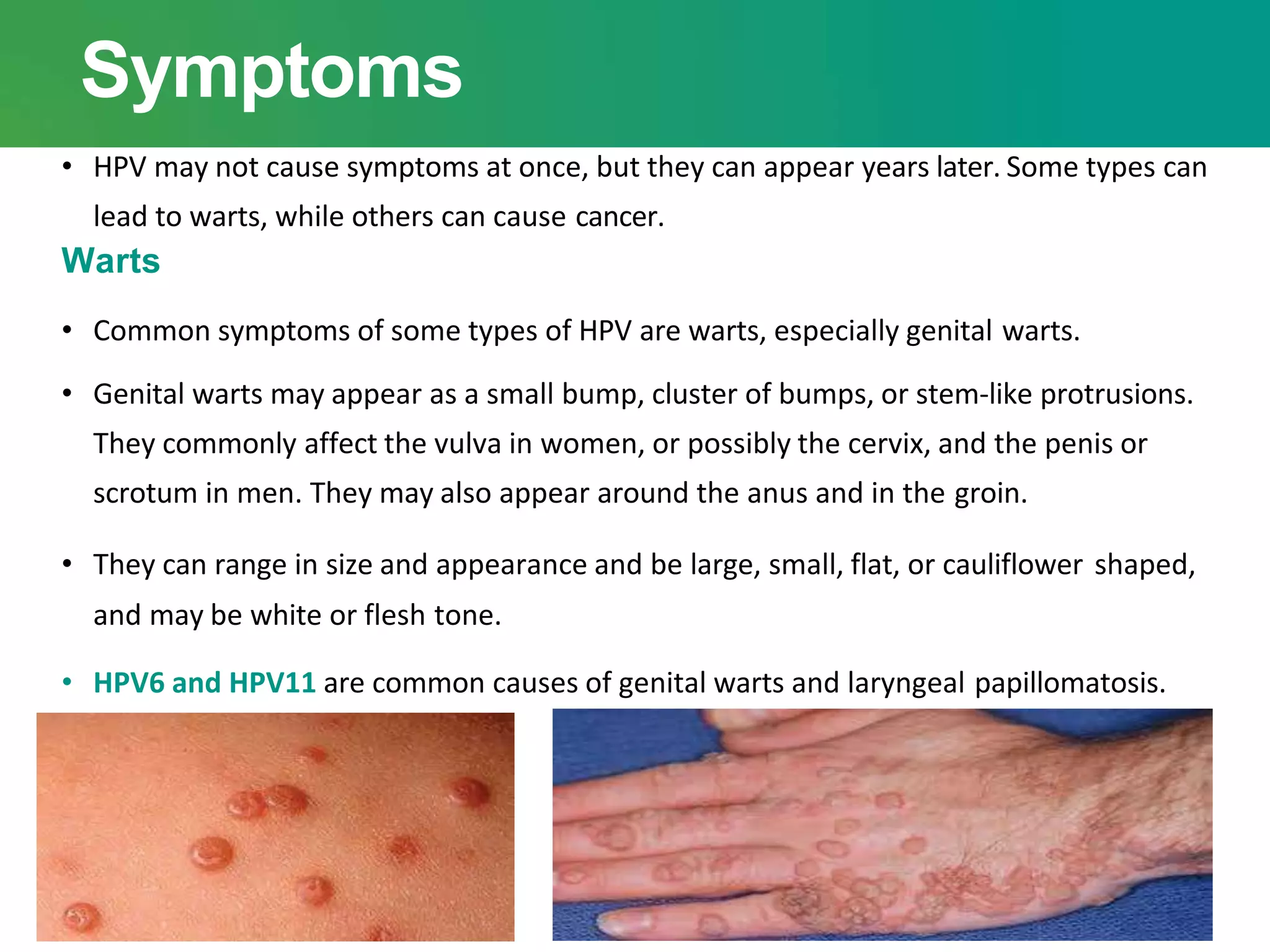
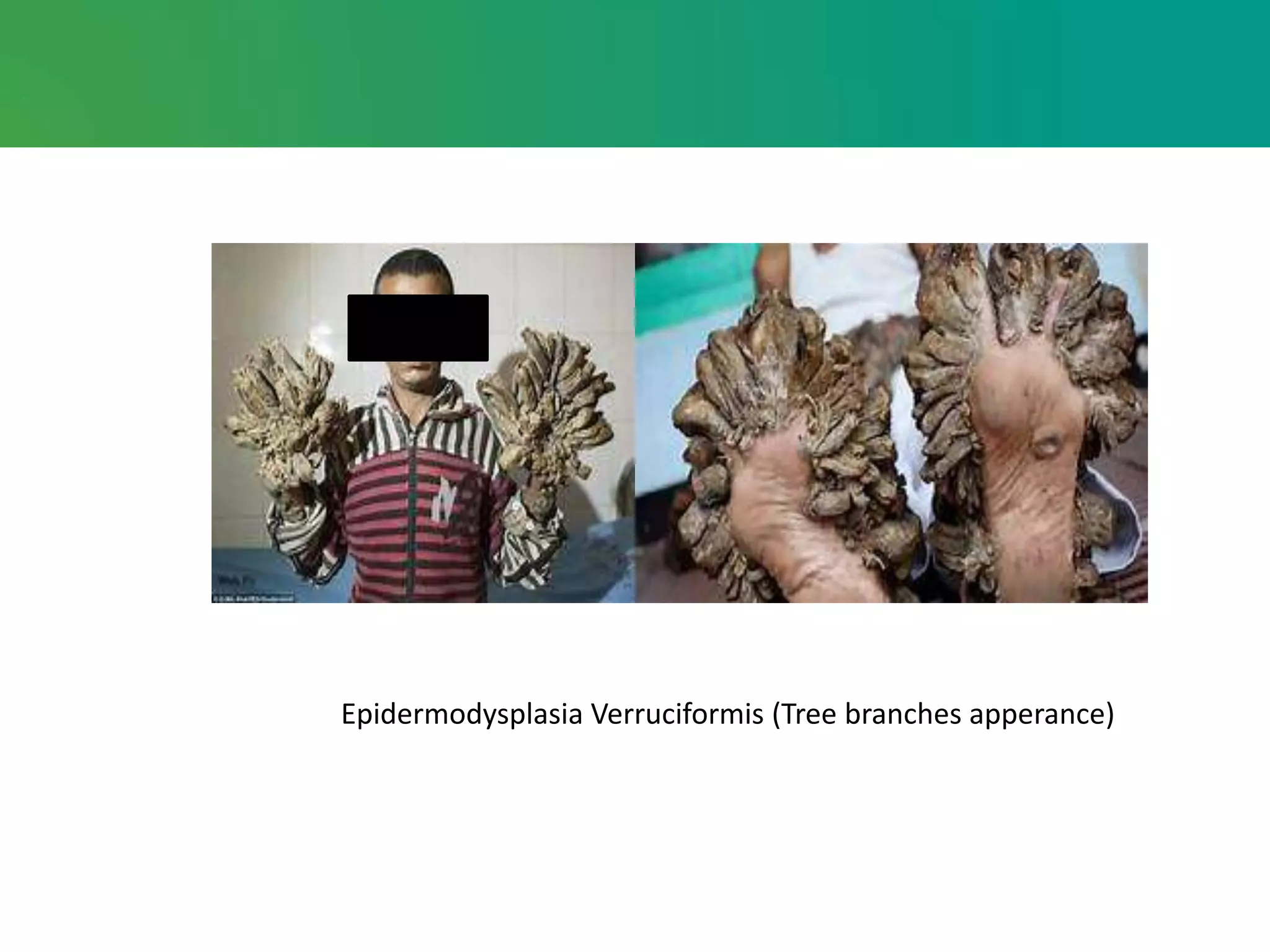
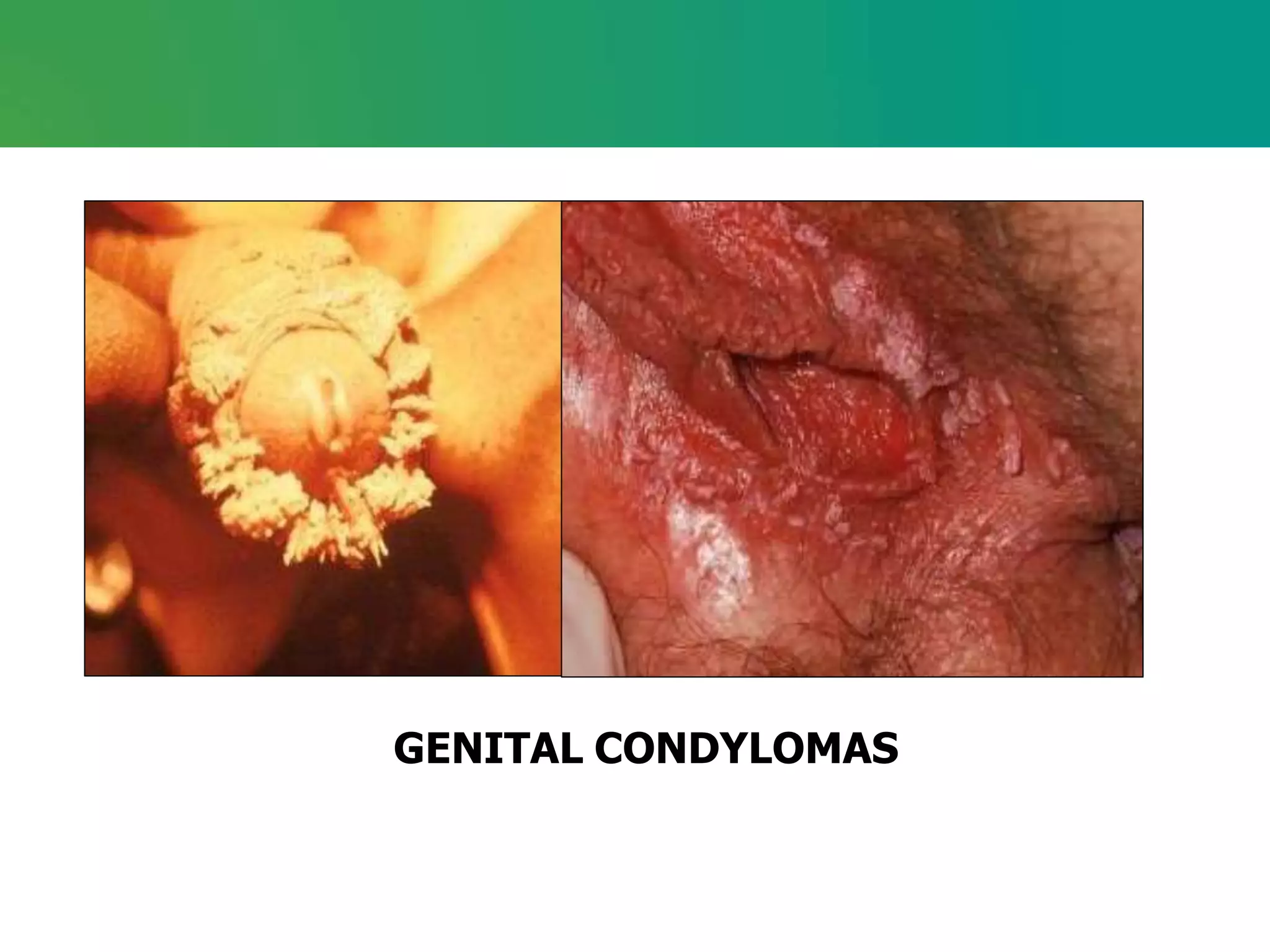
Human papillomavirus (HPV) is the most prevalent sexually transmitted infection, often showing no symptoms until years later, which can include genital warts or lead to various cancers, particularly cervical cancer. Transmission occurs through intimate skin-to-skin contact, and while most HPV infections resolve on their own, persistent infections may require diagnostic procedures like Pap smears or biopsies, and treatment options for warts include topical medications and surgical procedures. Vaccination is available to prevent HPV infections associated with cancer, and safer sexual practices can reduce the risk of transmission.