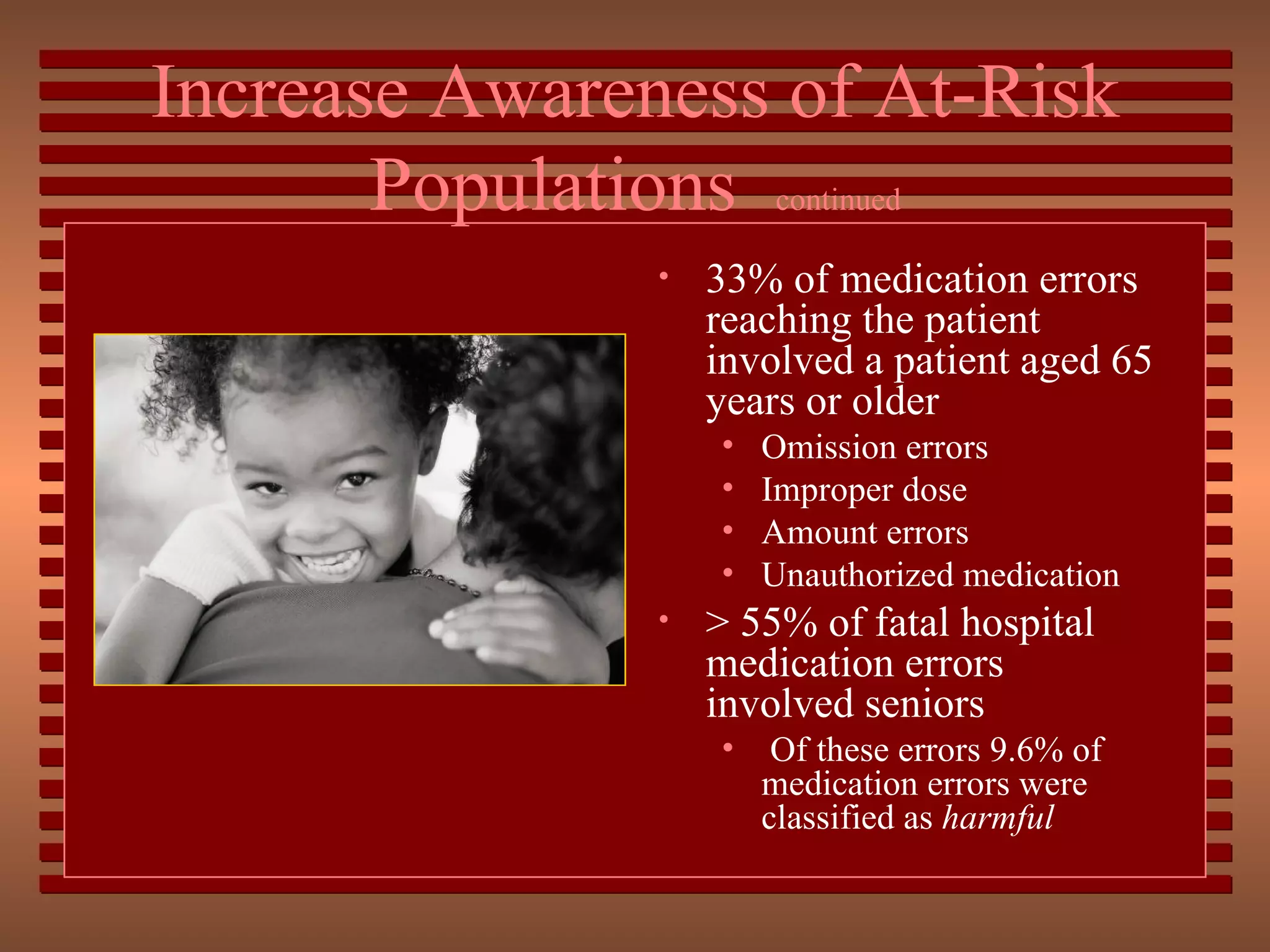
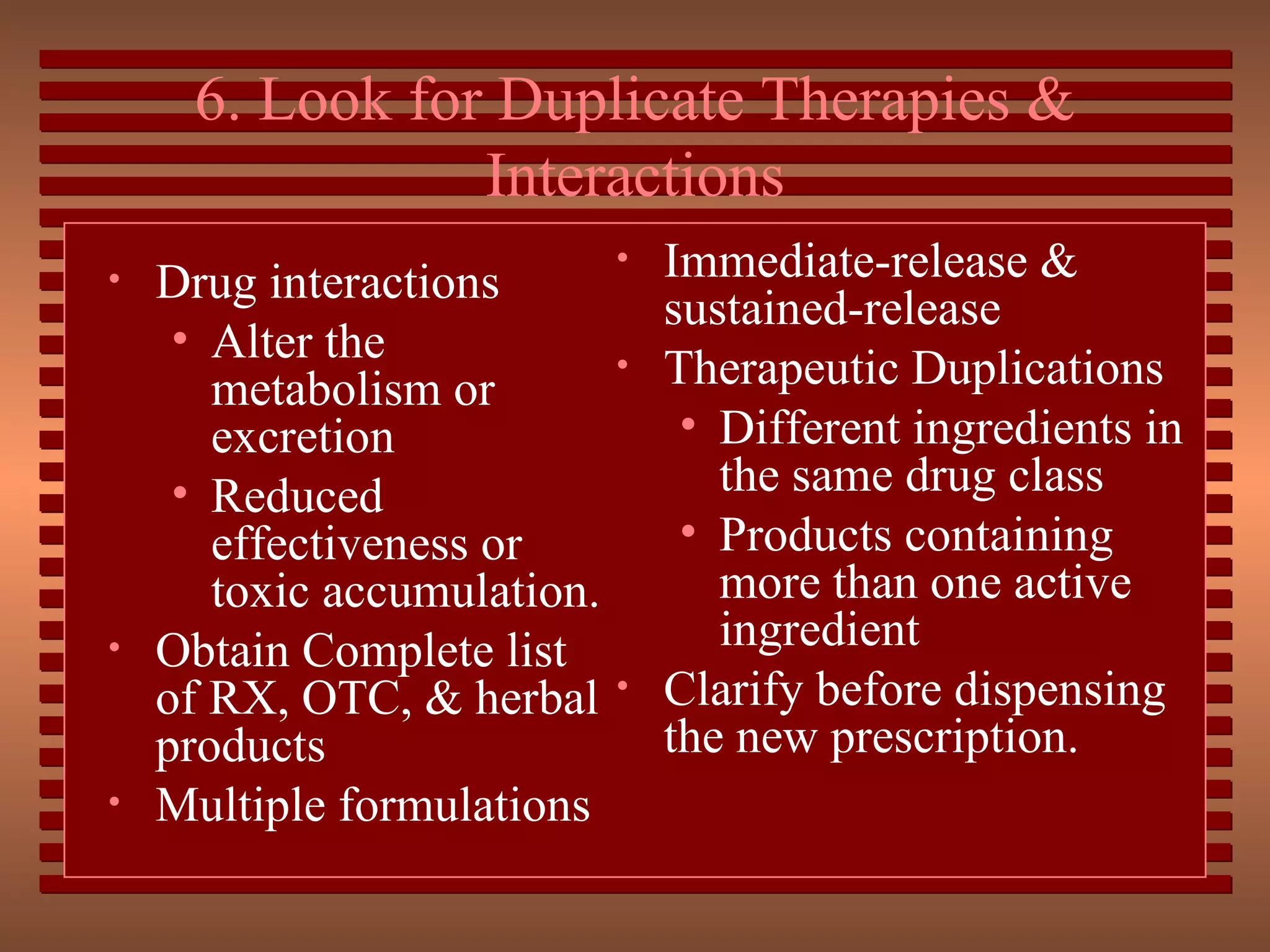
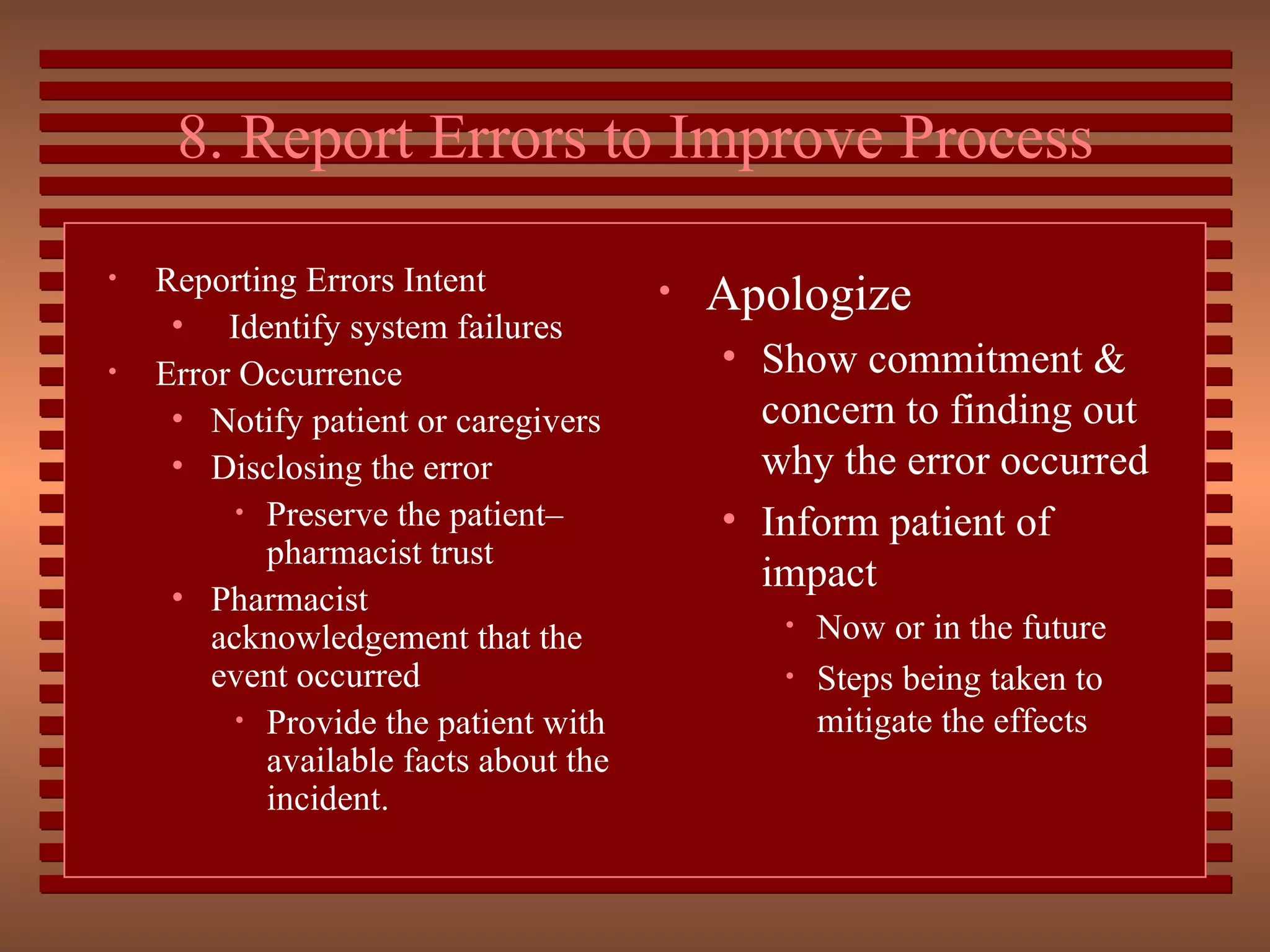
The document outlines several strategies to reduce medication errors, including increasing awareness of high-risk populations like pediatrics and geriatrics, avoiding abbreviations, recognizing look-alike and sound-alike medications, focusing on high-alert medications, reporting errors to improve processes, controlling the environment, and educating patients. It emphasizes the importance of a culture of safety, team approach, best practices, and technical support strategies to continuously improve patient safety.