This document provides an overview of the Stark Law, including:
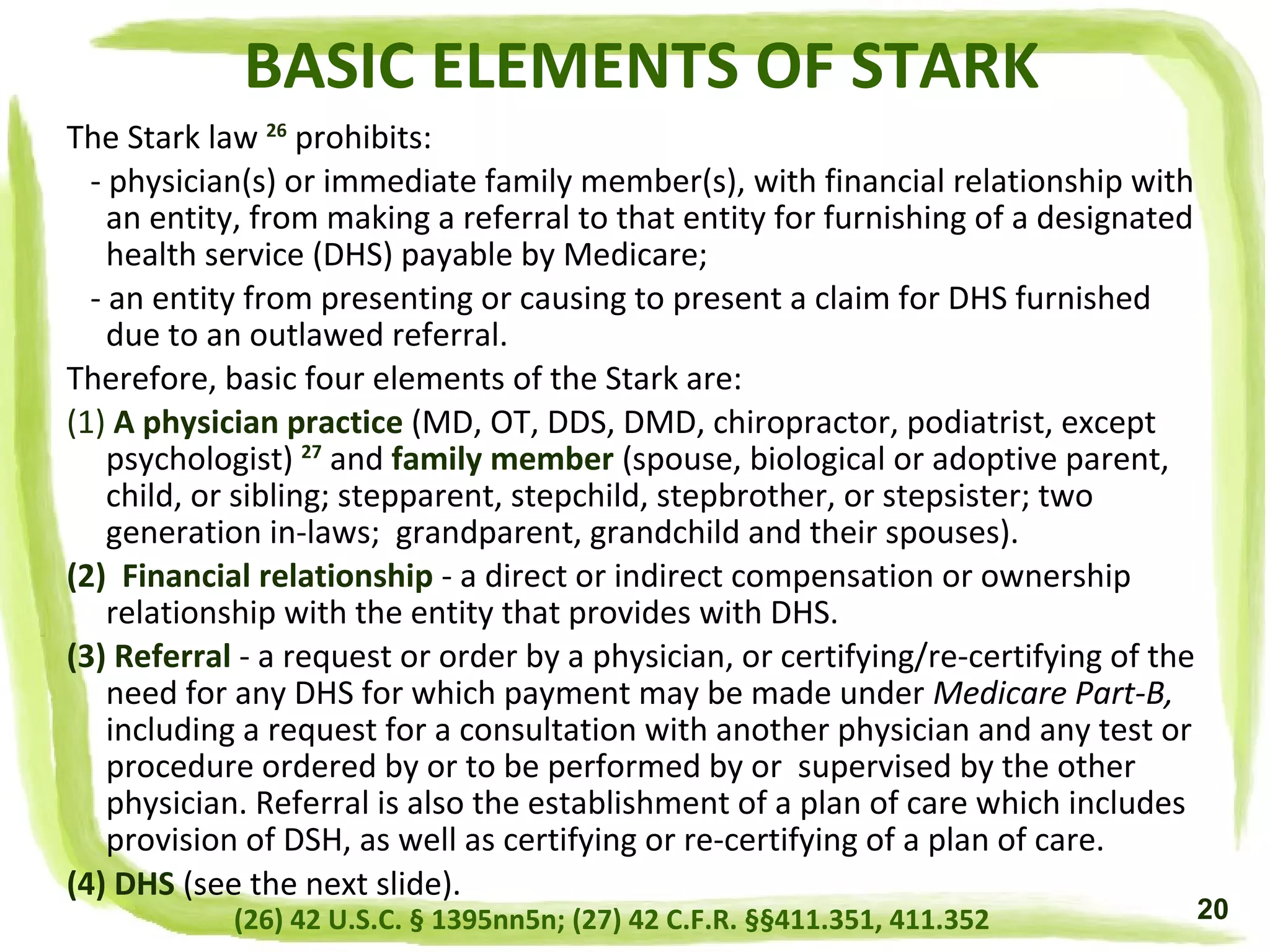
- The Stark Law prohibits physician self-referrals of Medicare patients for designated health services if the physician has a financial relationship with the entity providing those services.
- It addresses questions about who enforces the law, why the law was created, what activities it prohibits, and differences between it, the Anti-Kickback Statute, and the False Claims Act.
- The document outlines penalties for Stark Law violations and lists 17 areas of compliance risk identified by the Office of Inspector General related to healthcare fraud and abuse.












































































![ELECTRONIC HEALTH RECORDS EXCEPTIONS
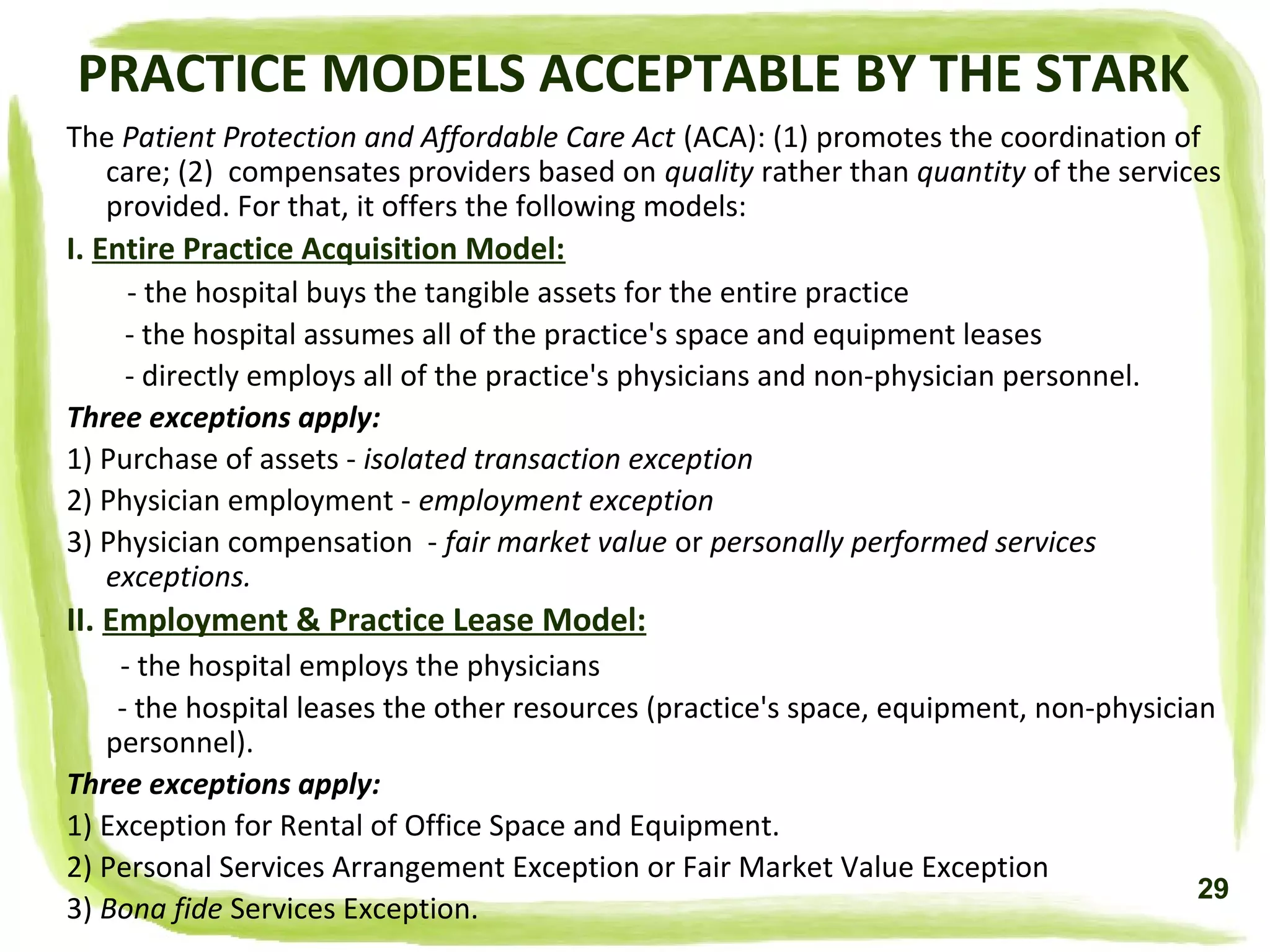
(1) E -prescribing Exception:
- the DHS entity may provide only hardware, software, or IT and training services that
are necessary and used solely for e-prescribing information
- it may not provide monetary remuneration
- e -prescribing items must be provided by:
[A] hospital to a physician who is a staff member;
[B] group practice to a member physician;
[C] Medicare Part-D sponsor or Medicare Advantage organization to a prescribing
physician;
[D] items and services must be provided in connection with an e-prescription drug
program that meets applicable standards under Medicare Part-D sponsor or Medicare
Advantage plan;
[E] do not restrict a physician's ability to use the items or services with other e-
prescribing or e-health records for any patient;
[F] a physician cannot make the receipt, amount or nature of items or services a
condition of doing business with the donor;
[G] eligibility of physician for items or services and nature or amount of items or
services can't take into account volume or value of referrals or other business;
[H] arrangement must be in a signed agreement that specifies:
- all items and services being provided
- donor's costs of items and services including all electronic prescriptions
- non monetary remuneration covering software or IT and training services needed
and is used to create, maintain, send or receive e-health records.
(93) 42 CFR Sec 411.357w
79](https://image.slidesharecdn.com/stark-160918234919/75/Stark-Law-by-Naira-Matevosyan-79-2048.jpg)























