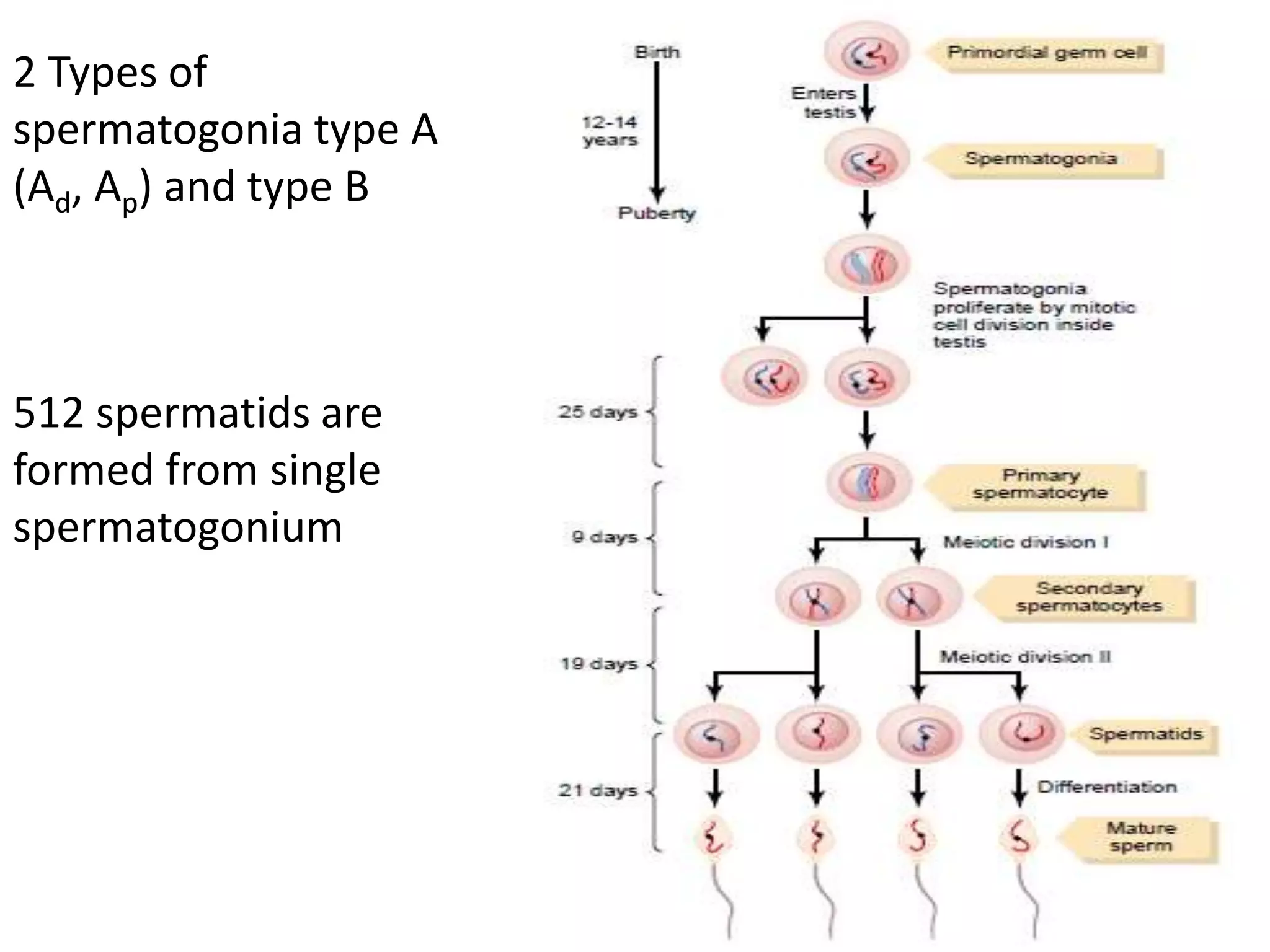
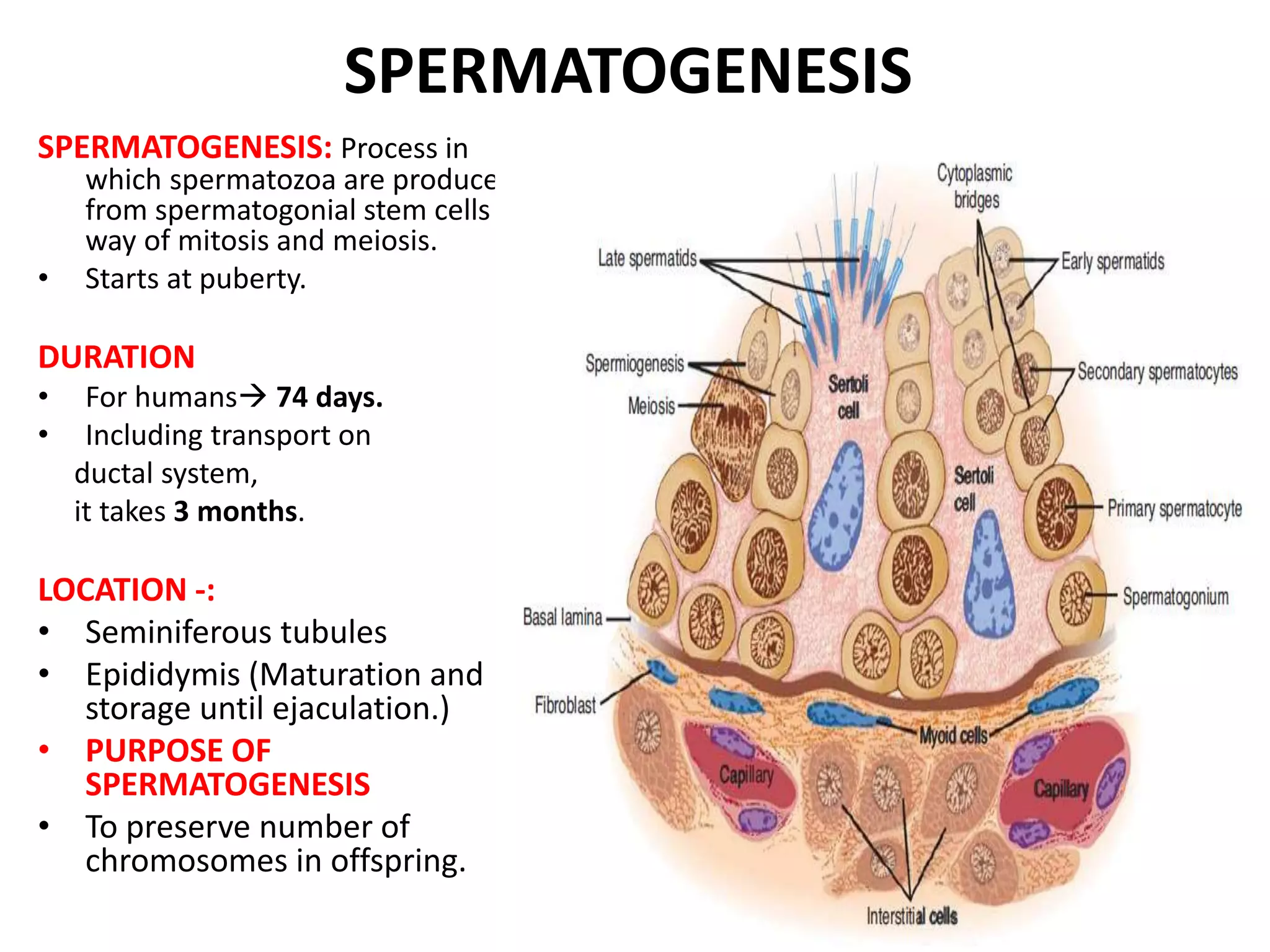
Spermatogenesis is the process by which sperm are produced in the testes. It begins at puberty and takes approximately 74 days to complete. It occurs in the seminiferous tubules of the testes and involves the transformation of spermatogonia stem cells through meiosis into mature sperm. Sertoli cells provide nourishment and structural support during spermatogenesis. Hormones such as testosterone and FSH control spermatogenesis. Abnormalities in spermatogenesis can lead to male infertility.














![OTHER FACTORS AFFECTING SPERMATOGENESIS
Temperature:
• Seminiferous epithelium is sensitive to elevated temperature as high as
normal body temperature. Consequently, in scrotum. The optimal
temperature is maintained at 2 °C below body temperature.[ Achieved by
regulation of blood flow ]
• Scrotal reflex: Positioning towards and away from the heat of the body by
cremasteric muscle and Dartos smooth muscle in scrotum.
Others-:
• Dietary deficiencies (such as vitamins B, E and A), infectious diseases.
• Anabolic steroids , metals (cadmium and lead), x-ray exposure, dioxin,
alcohol, pesticides .
• DNA damage caused by oxidative stress.](https://image.slidesharecdn.com/spermatogenesis-171112112558/75/Spermatogenesis-17-2048.jpg)



![FUNCTIONS OF TESTOSTERONE
In fetal period -:
• Genital ridges secretes testosterone [& estrogens]
• fetal testes starts secretion @ 7 week
• Causes genital differentiation (wolffian duct)
• Differentiation of external genitalia
• Suppress formation of female genital organs (mullerian duct)
What happens if ?
• Injection of male sex hormones in large quantities in pregnant
animals having female fetus ?
• Removal of male testis in early male fetus ?
Effect of testosterone on descent of testis:
• Usually descend in last 2-3 months of gestation in to the scrotum](https://image.slidesharecdn.com/spermatogenesis-171112112558/75/Spermatogenesis-22-2048.jpg)



![SPERM COUNT ABNORMALITIES
Normal count 120 million/ml [< 20 million/ml sterile]
Aspermia: Absence of semen
Azoospermia: absence of sperm
Hypospermia: low semen volume
Hyperspermia: high semen volume
Oligozoospermia: Very low sperm count
Asthenozoospermia: poor sperm motility
Teratozoospermia: sperm carry more morphological defects than
usual
Necrozoospermia: all sperm in the ejaculate are dead
Leucospermia: a high level of white blood cells in semens
(>1 million/cc)](https://image.slidesharecdn.com/spermatogenesis-171112112558/75/Spermatogenesis-26-2048.jpg)