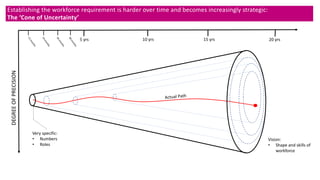
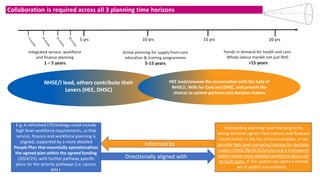
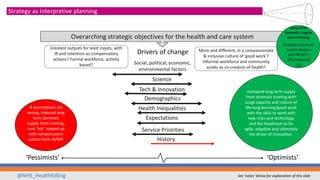
This document outlines plans to create a long-term strategic framework for the health and social care workforce in England. It will include regulated professionals working in adult social care for the first time. The framework will look at key drivers of workforce demand and supply over the long term to identify strategic choices and required actions. This will require collaborating with partners from all levels and sectors to build shared goals and assumptions to guide more detailed workforce plans nationally and locally. Achieving the required expertise can take over a decade, so workforce investment must consider needs for both the present and future.