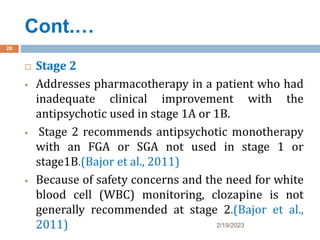
The document discusses the pharmacotherapy of schizophrenia. It begins by outlining the objectives of recognizing symptoms, explaining pathophysiology, identifying treatment goals, and comparing antipsychotic medications. It then covers the introduction, etiology, types, pathophysiology, signs and symptoms, and management of schizophrenia including current practices. Management involves psychosocial interventions, medications, and ECT. Treatment is divided into acute, stabilization, and maintenance phases. The document provides recommendations for antipsychotic selection and monitoring side effects. It acknowledges controversies around first-generation versus second-generation antipsychotics and long-acting injections.





























![CONTROVERSY
2/19/2023
32
With the introduction of SGAs in the 1990s, the use of
FGAs has progressively decreased, and FGAs have less than
10% market share of the antipsychotics used for
schizophrenia.
This decline occurred because of the touted better side
effect profile and other possible benefits of SGAs in
nonpsychotic domains of the illness.
However, a large landmark study (the Clinical
Antipsychotics Trials of Intervention Effectiveness [CATIE
trial]; The study revealed that the FGA was equal to the
SGAs for the primary endpoint of time to discontinuation
of medication. (Lieberman et al., 2005)](https://image.slidesharecdn.com/schizo-230219114946-bf123de5/85/schizo-pptx-32-320.jpg)




