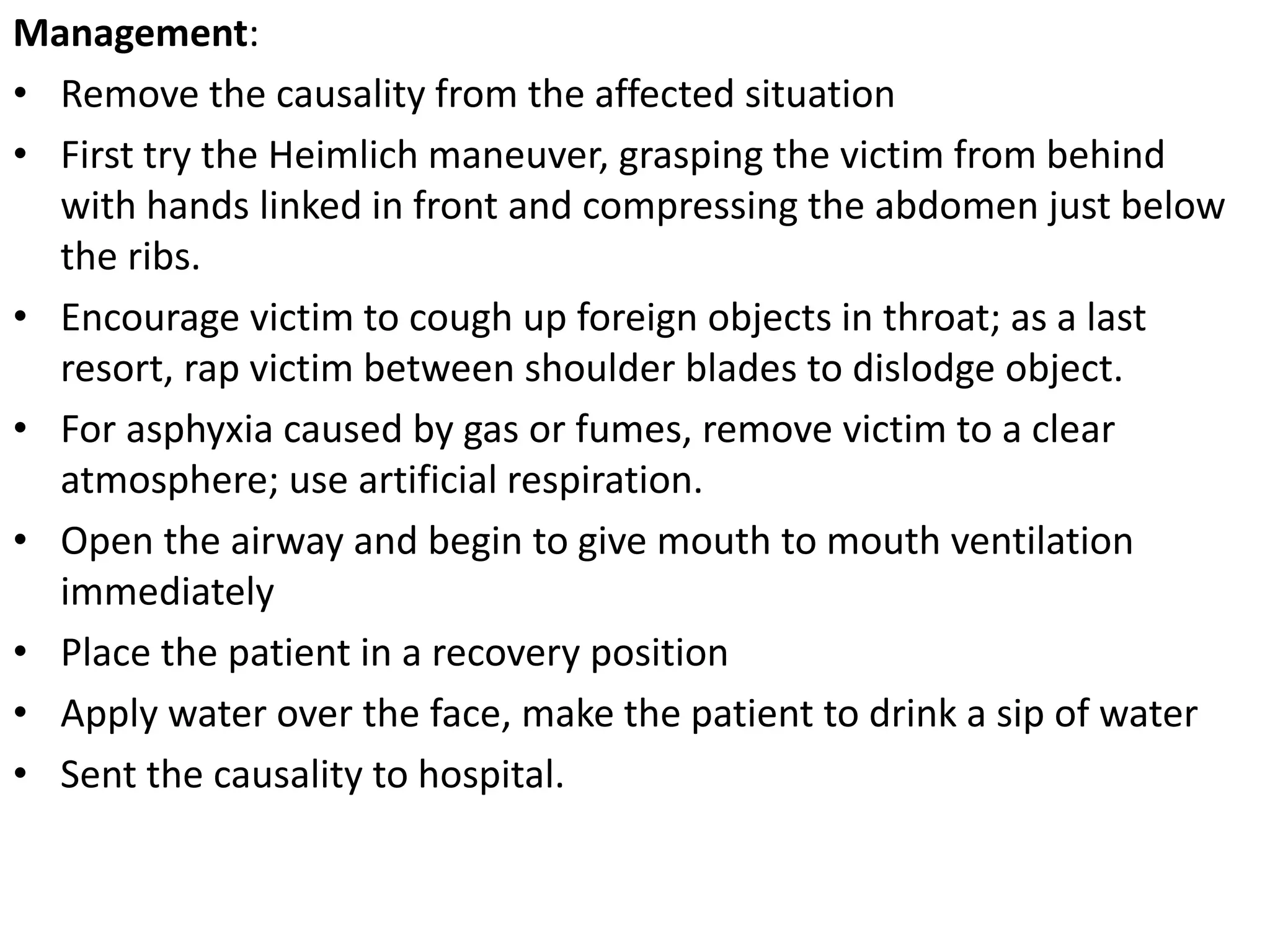
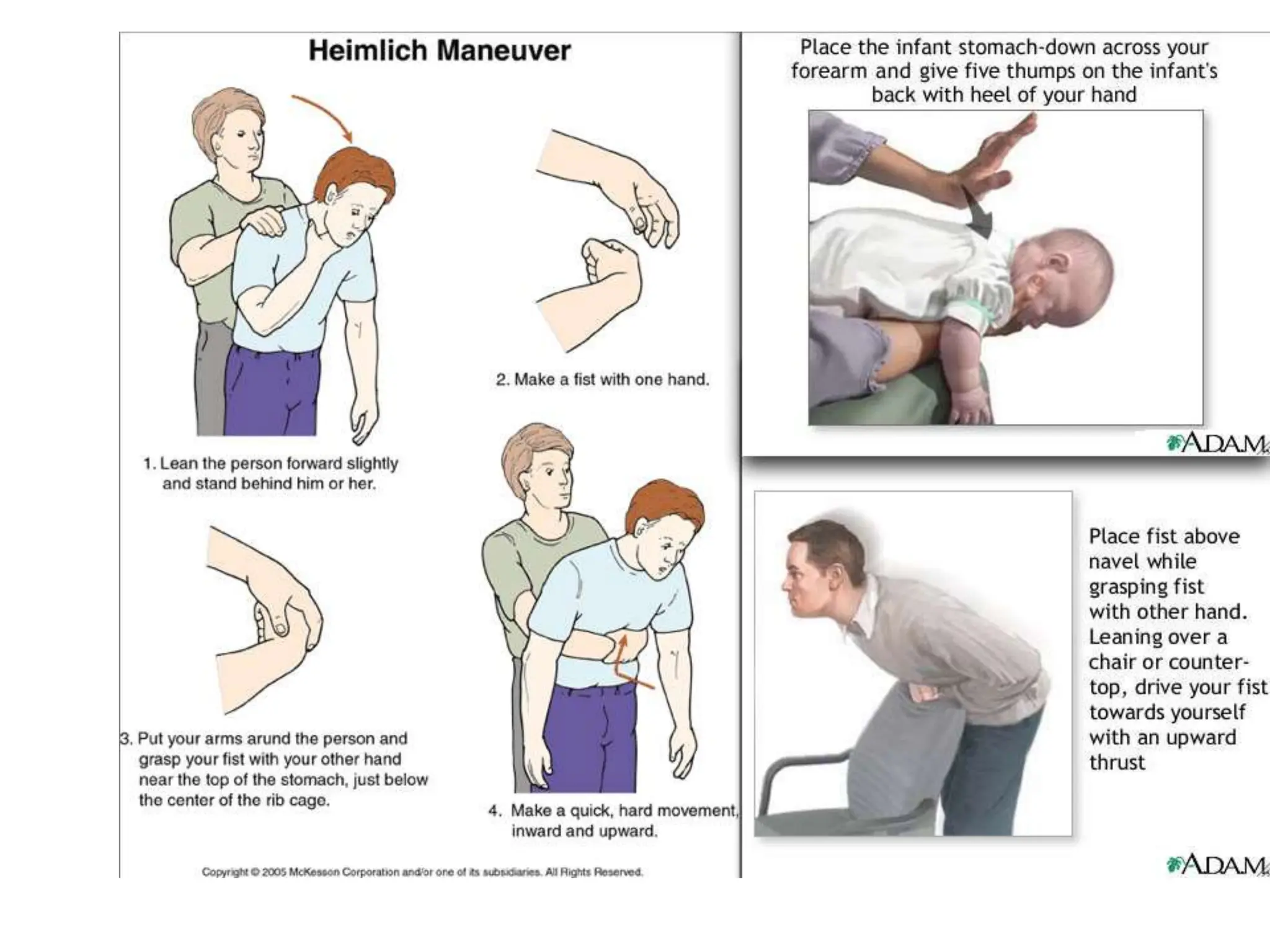
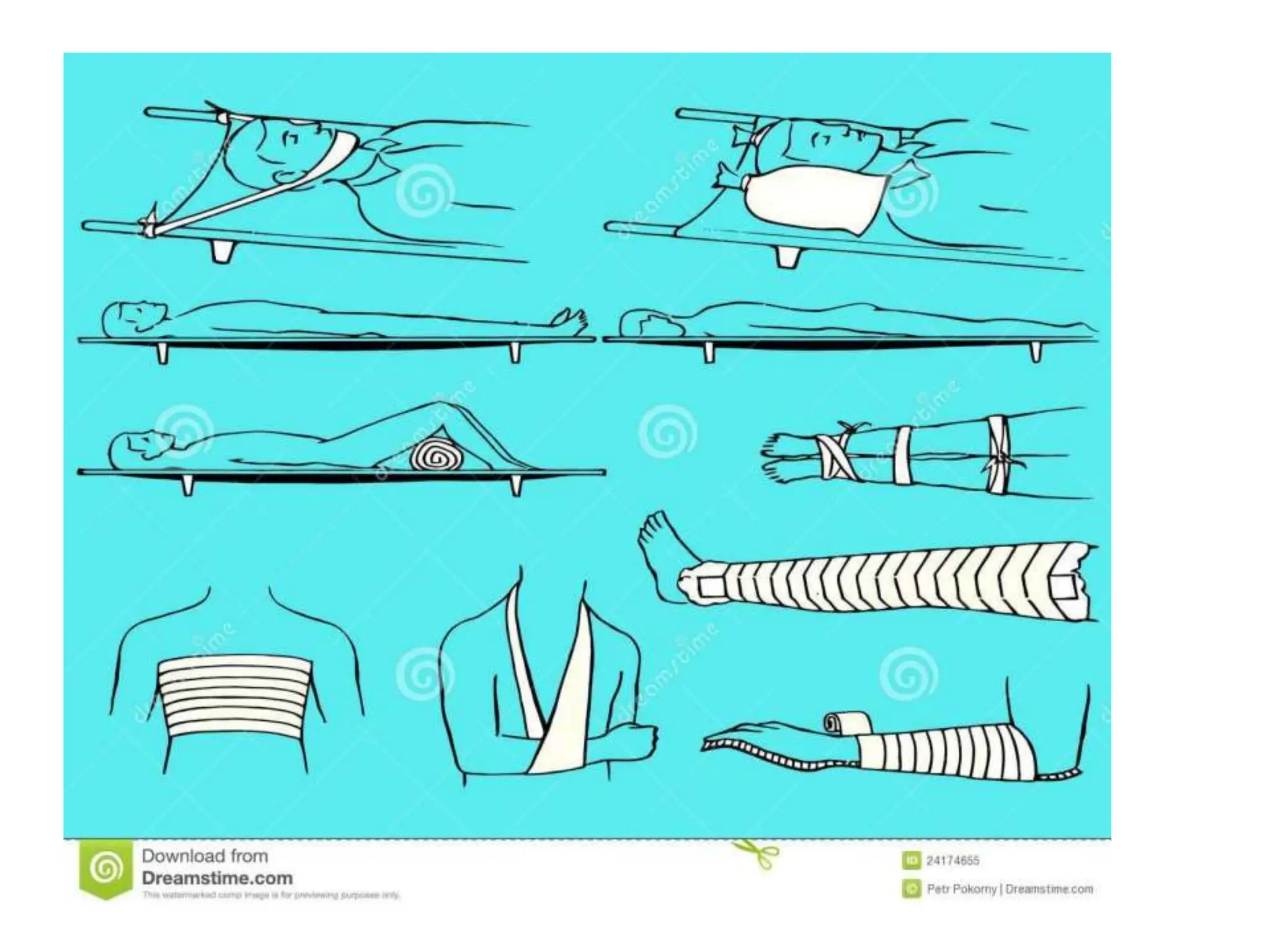
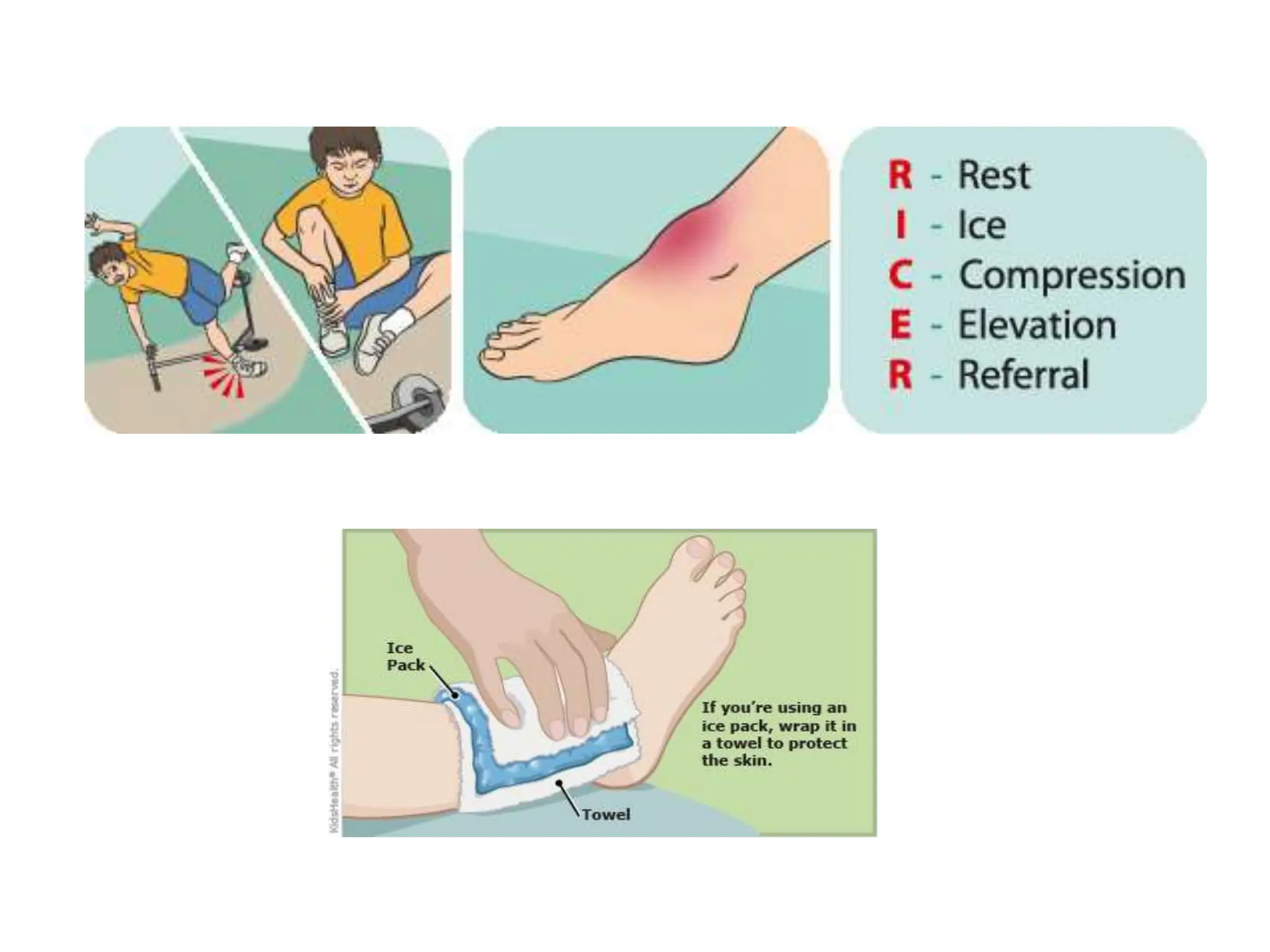
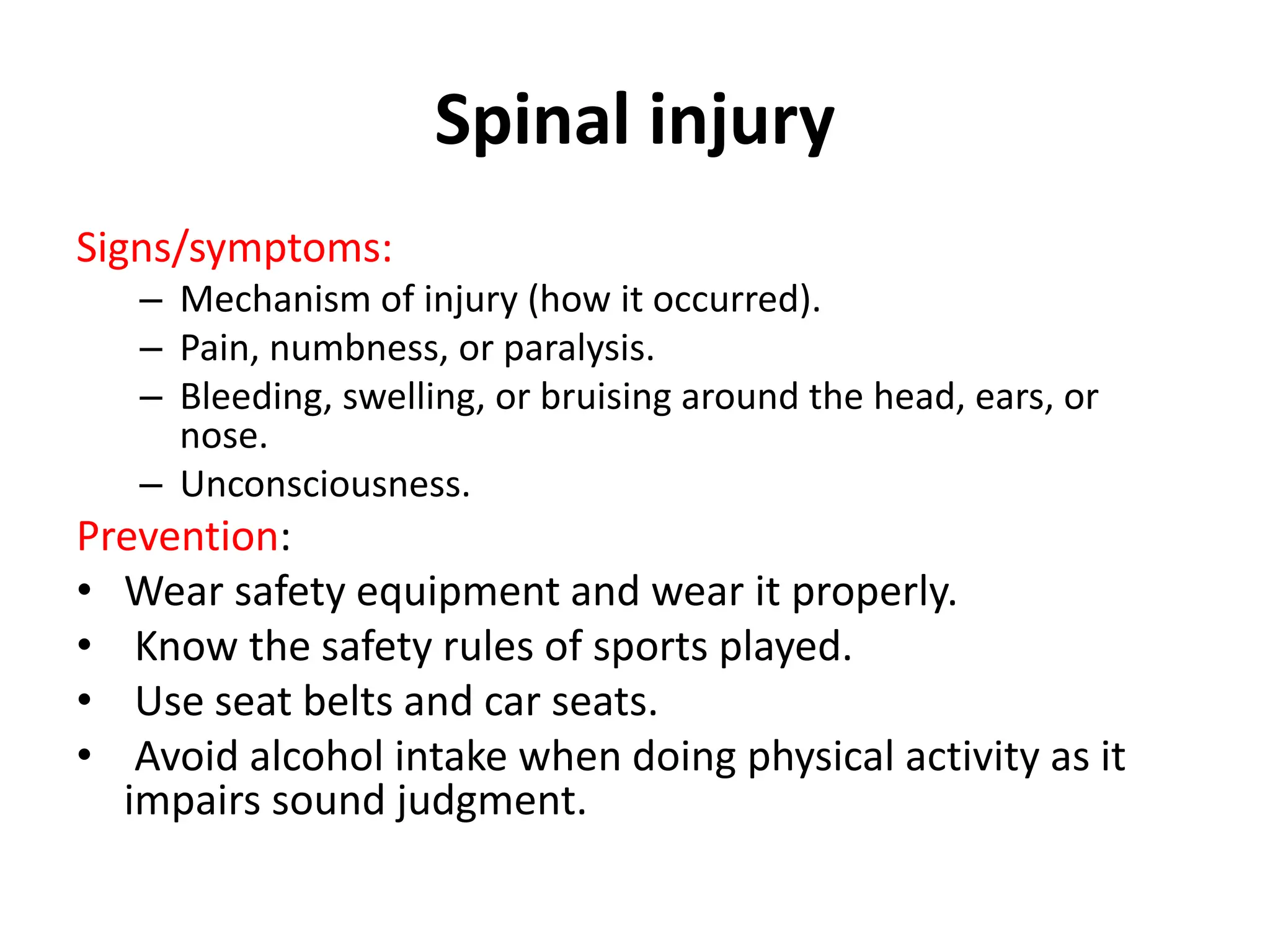
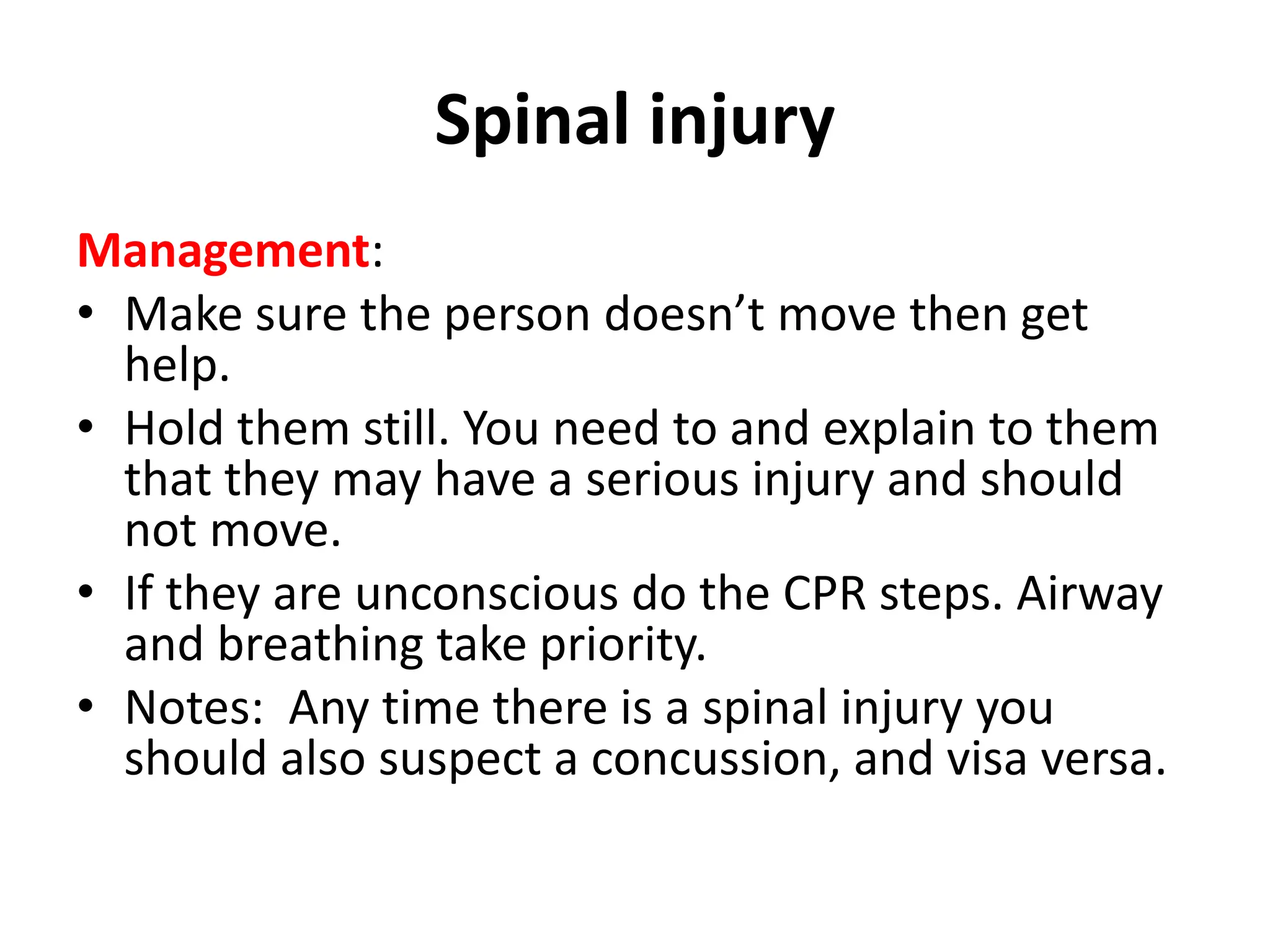
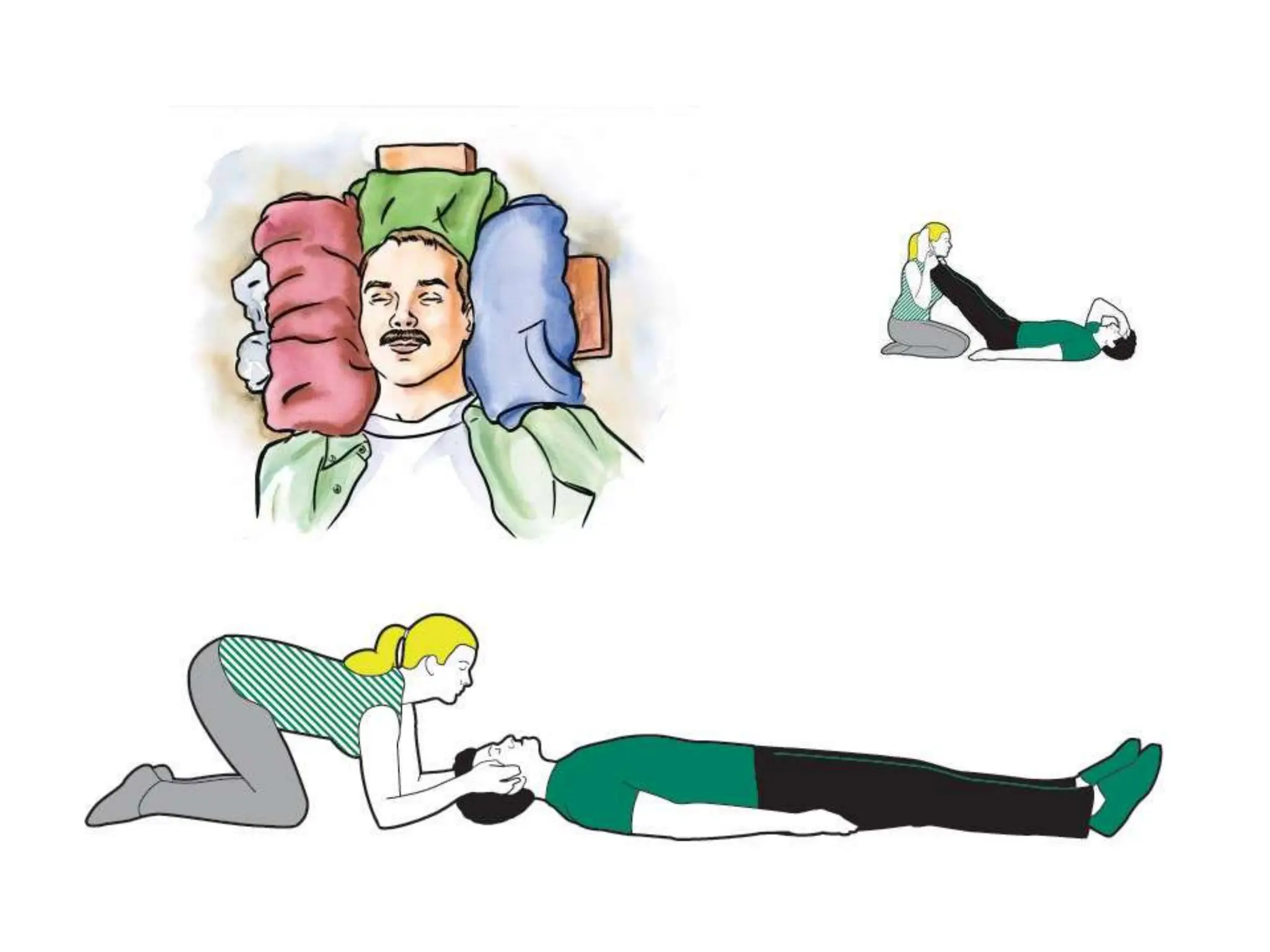
First aid is the initial support provided to individuals suffering from injuries or illnesses until professional medical help arrives. Key principles include maintaining airway, breathing, and circulation, as well as addressing specific emergencies like asphyxia, drowning, and bleeding. Basic knowledge of first aid is crucial in emergencies to potentially save lives and improve recovery outcomes.