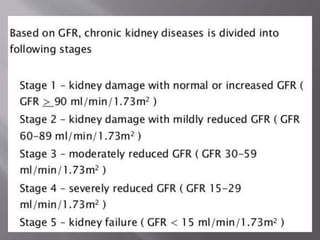
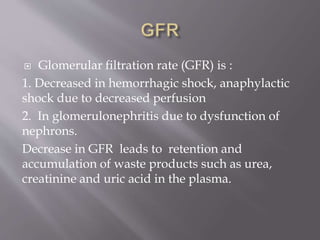
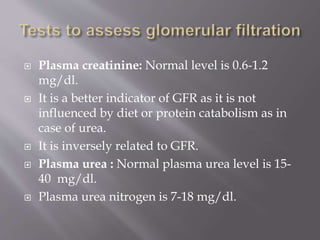
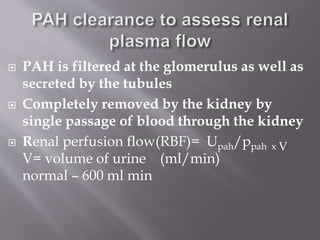
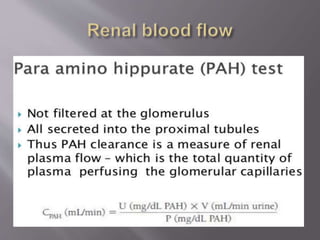
The document discusses renal function tests, their purposes in diagnosing and monitoring kidney health, and describes key parameters such as glomerular filtration rate (GFR) and creatinine clearance. It emphasizes the significance of various substances, including urea, creatinine, and cystatin C, as indicators of renal function, along with the impact of renal diseases on these markers. Additionally, it reviews urine characteristics and abnormalities that can indicate kidney dysfunction, including proteinuria and specific gravity variations.
![ GFR mL/minute = [(140 – age in
years) × (wt, kg)]/ 72 × P (mg/L) ×
0.85 (if subject is female).
If converting to SI units (GFR in
micromoles per liter) is desired,
replace 72 in the denominator with
0.84.](https://image.slidesharecdn.com/renalfunctiontests-200525115338/85/Renal-function-tests-19-320.jpg)
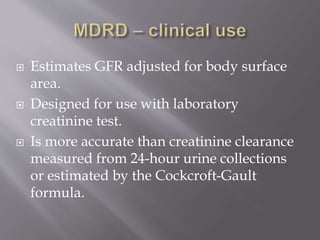
![ GFR (mL/minute/(1.73 m2)) = 186
× (serum creatinine [mg/dL]–1.154)
× (age in years)-0.203 × (0.742 if
female) × (1.210 if
African American).
If converting to SI units (GFR in
micromoles per liter) is desired,
replace 186 with 32,788.](https://image.slidesharecdn.com/renalfunctiontests-200525115338/85/Renal-function-tests-20-320.jpg)