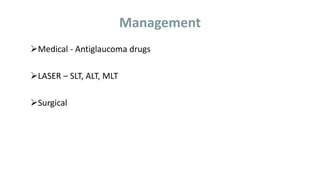
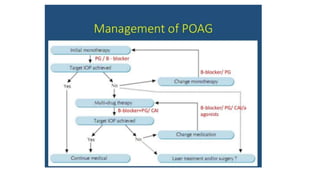
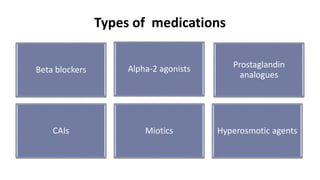
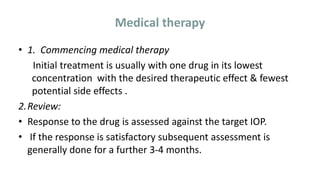
Primary open-angle glaucoma (POAG) is characterized by elevated intraocular pressure, glaucomatous optic nerve damage, and an open anterior chamber angle. It is the most common type of glaucoma and risk factors include older age, family history, and elevated eye pressure. The goal of treatment is to lower eye pressure through medications, laser therapy, or surgery in order to slow the progression of vision loss and prevent blindness. Regular eye exams are important for screening and monitoring the disease.