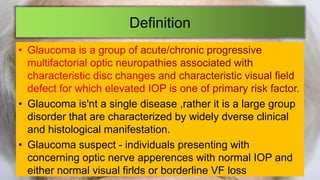
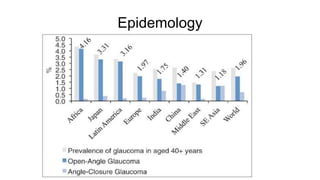
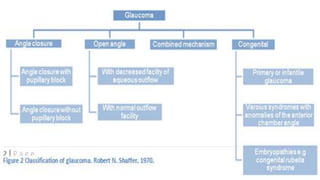
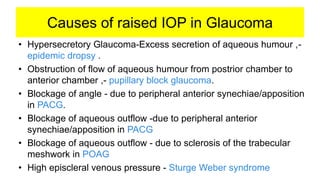
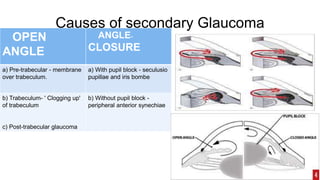
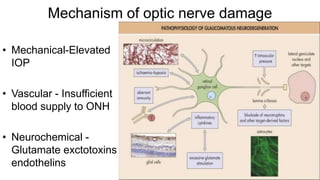
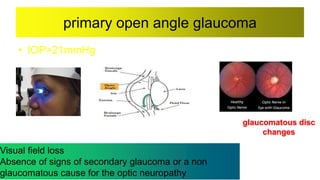
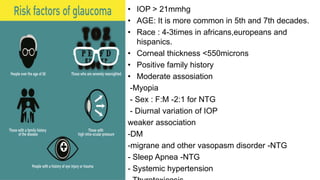
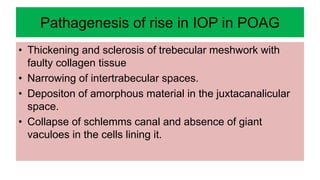
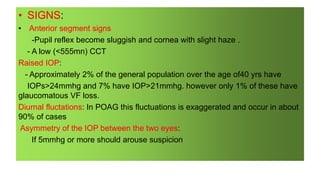
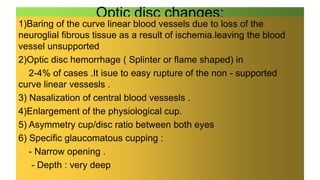
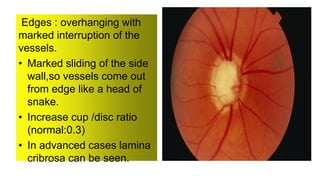
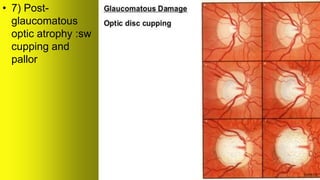
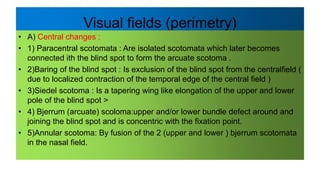
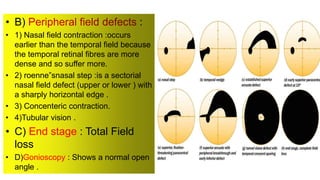
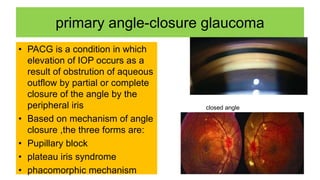
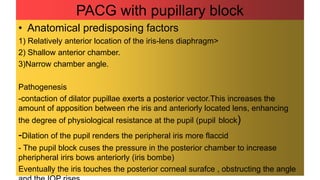
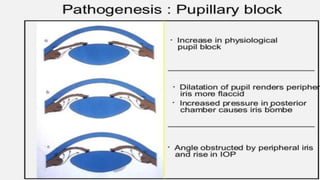
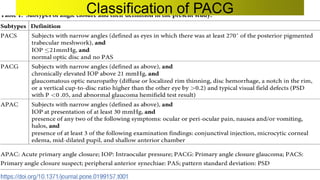
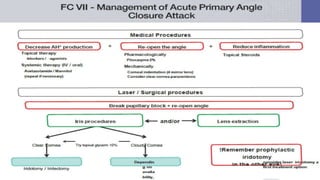
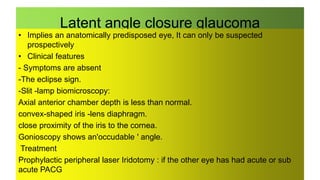
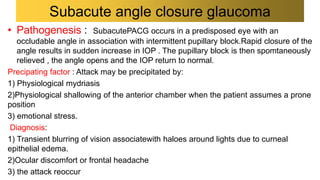
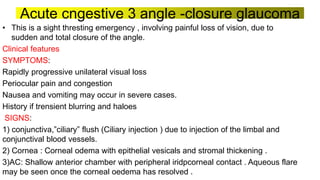
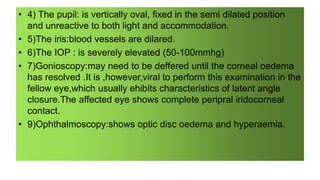
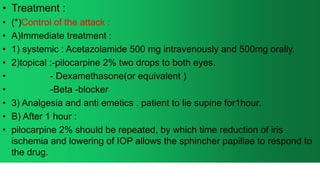
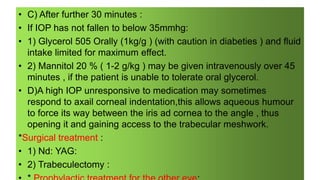
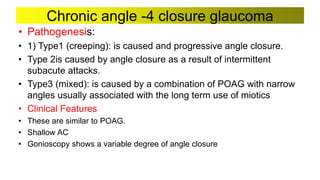
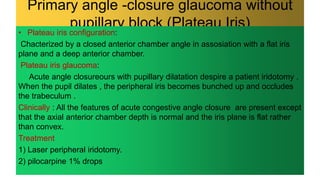
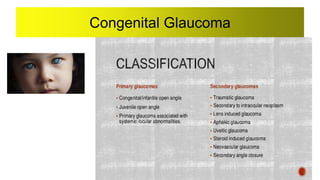
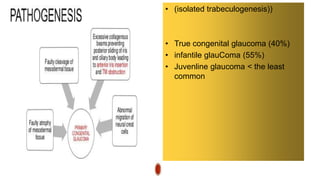
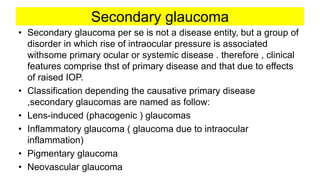
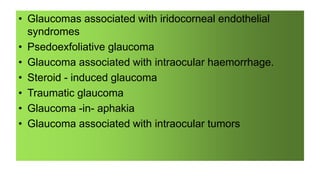
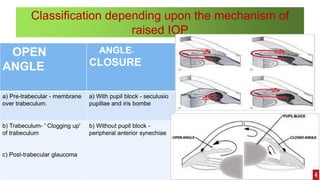
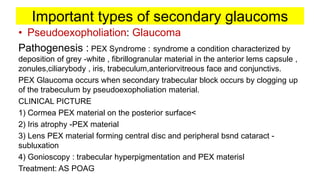
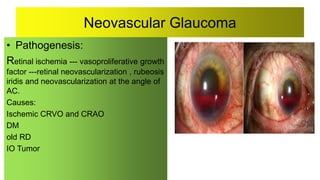
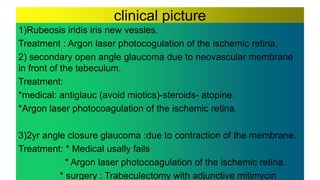
Glaucoma is a group of eye disorders characterized by optic nerve damage and vision loss caused by increased pressure in the eye. The document discusses the definition, epidemiology, causes, clinical features, diagnosis, and management of primary open angle glaucoma and primary angle-closure glaucoma. Key points include that glaucoma has various clinical manifestations, causes include blockage of aqueous outflow, signs involve optic nerve changes and visual field loss, and treatment aims to lower intraocular pressure through medication, laser treatment, or surgery.