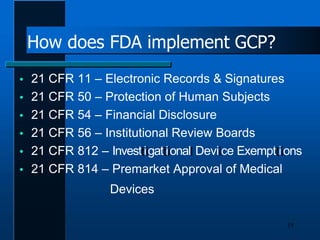
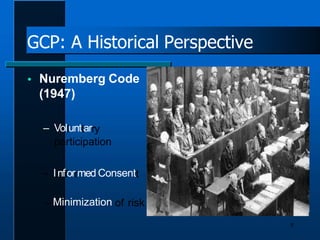
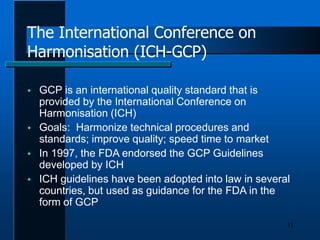
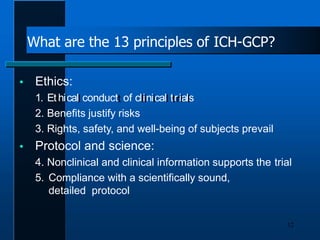
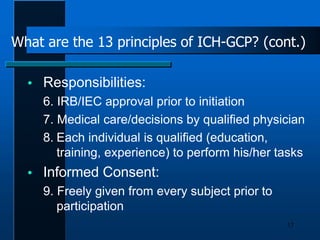
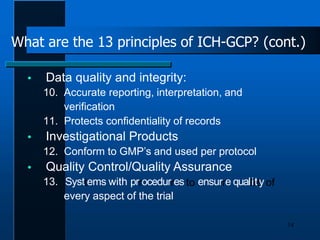
Good Clinical Practice (GCP) establishes international standards for conducting clinical research ethically and producing reliable data. GCP originated from documents like the Nuremberg Code and Declaration of Helsinki to protect subjects. The International Conference on Harmonisation further developed 13 principles for GCP covering ethics, scientific conduct, responsibilities, and quality assurance. FDA regulations implement GCP for medical device research to assure rights, safety, and data integrity.





![What constitutes Good Clinical
Practice in device research?
17
IRB-approved protocol
Valid Informed Consent
Monitoring Plan
Adverse Device Effect Reporting [Adverse
Event (AE) or Serious Adverse Event (SAE)]
Proper documentation
Valid data collection/reporting procedures](https://image.slidesharecdn.com/presentation-good-clinical-practice-101-an-introduction-pdf-version-211017163740/85/Presentation-good-clinical-practice-101-an-introduction-pdf-version-17-320.jpg)