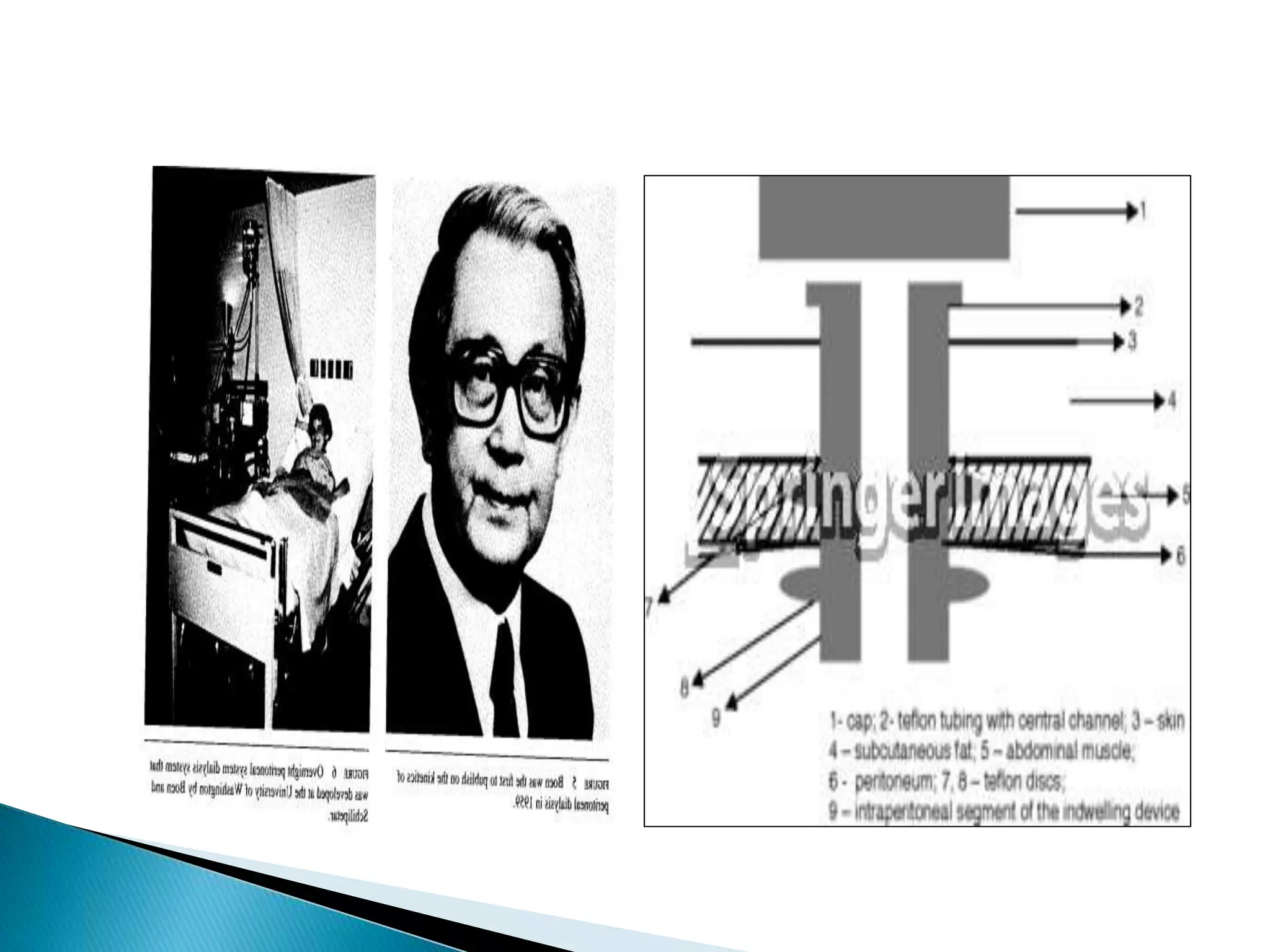
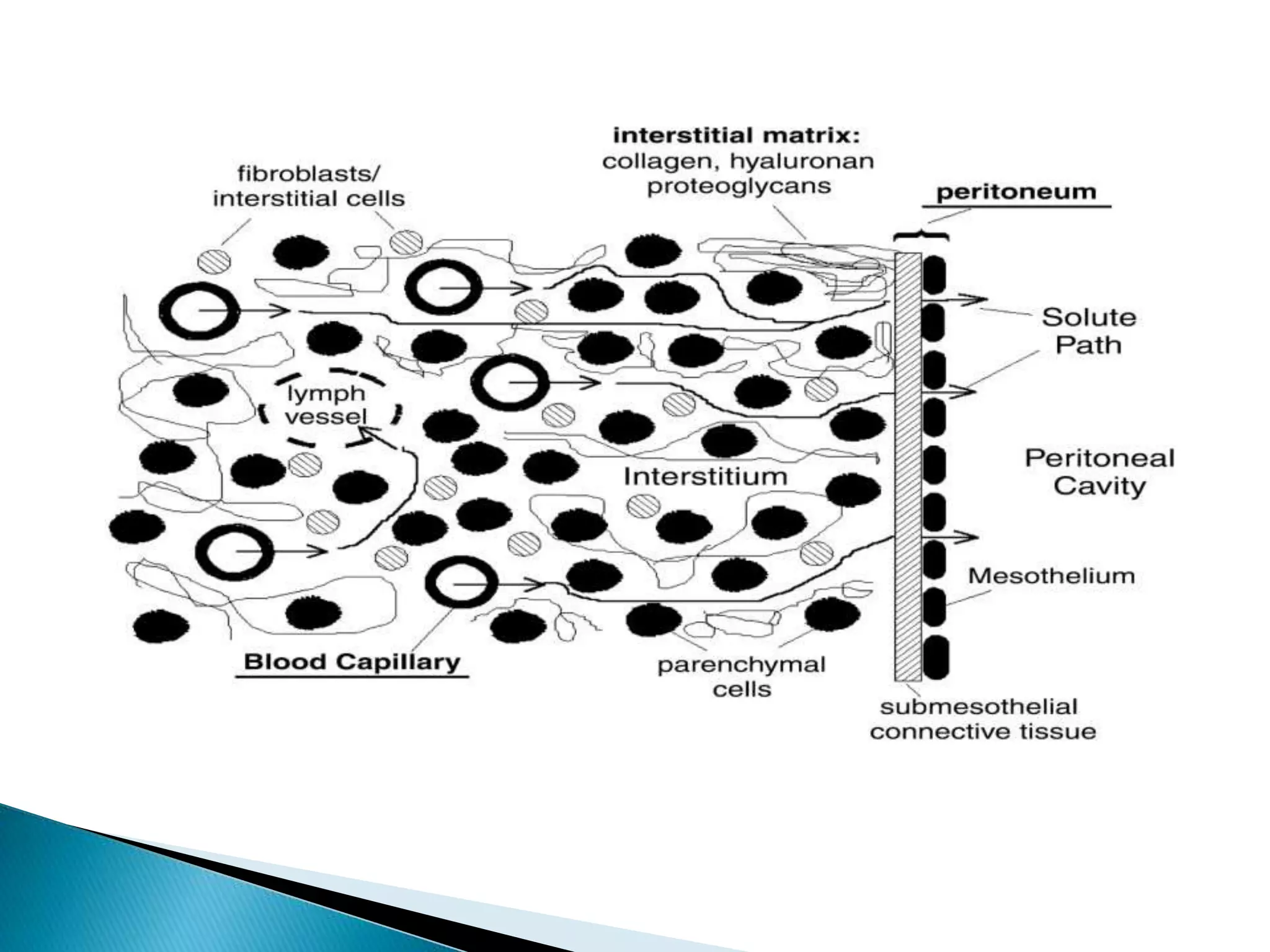
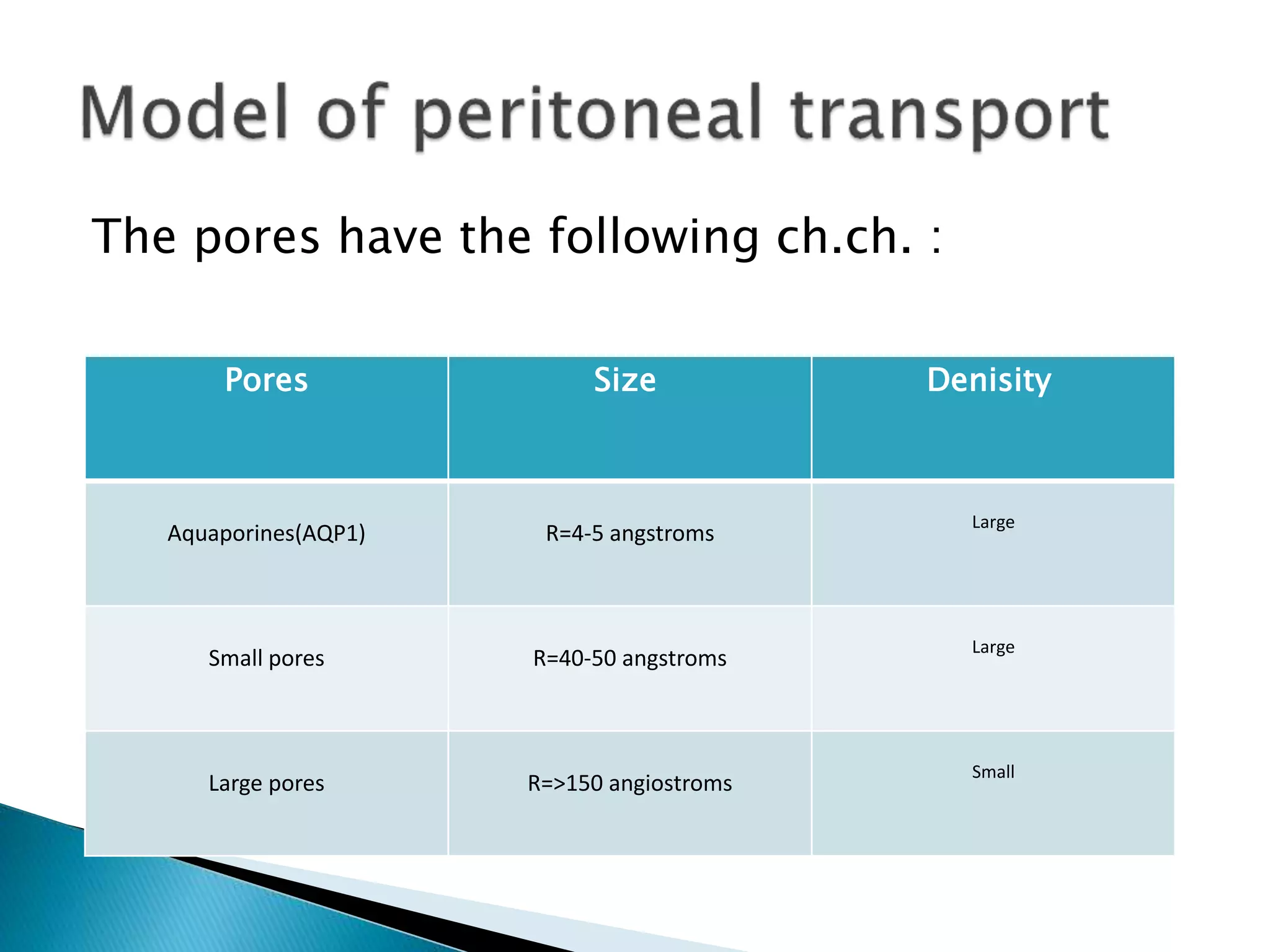
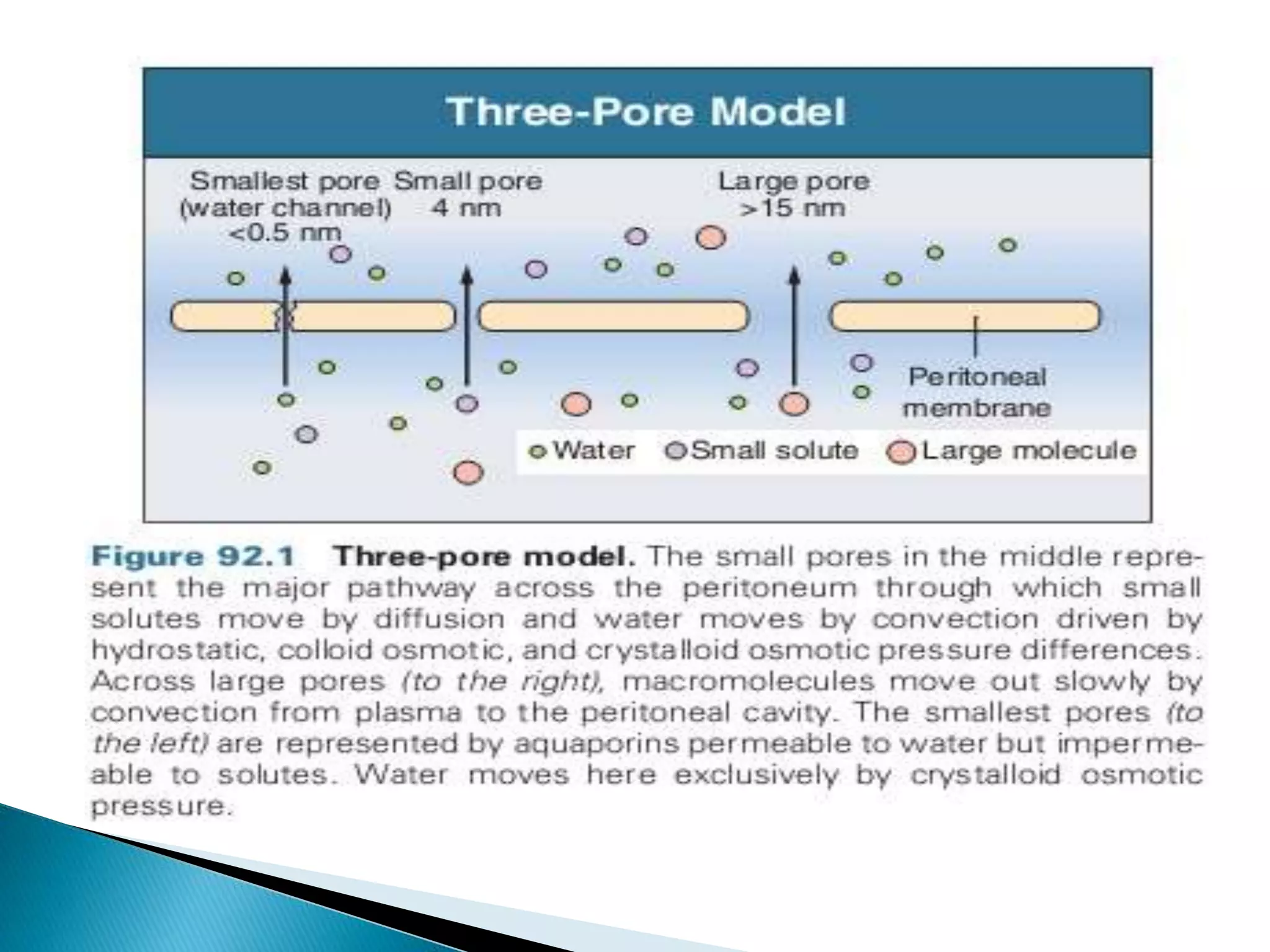
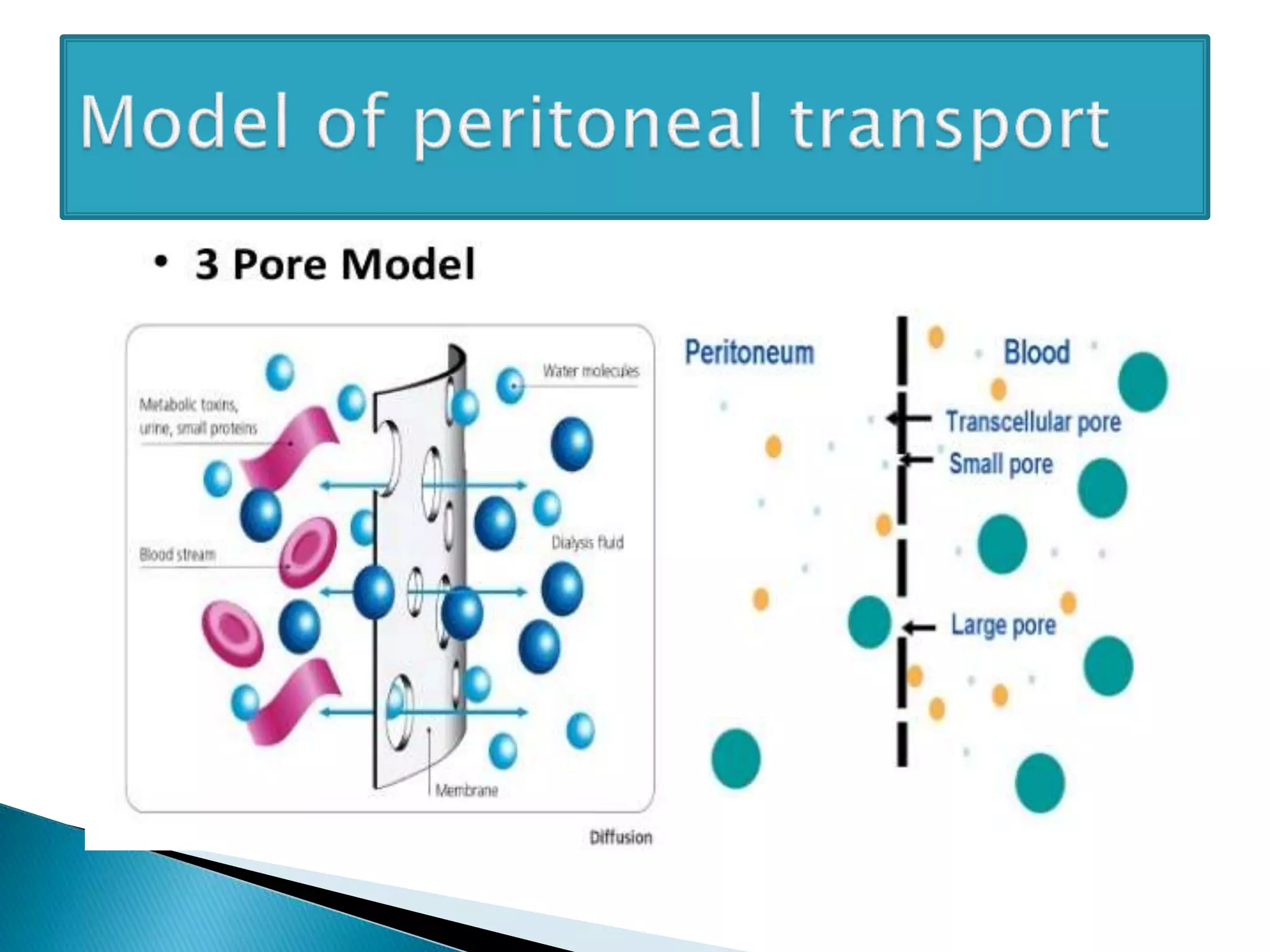
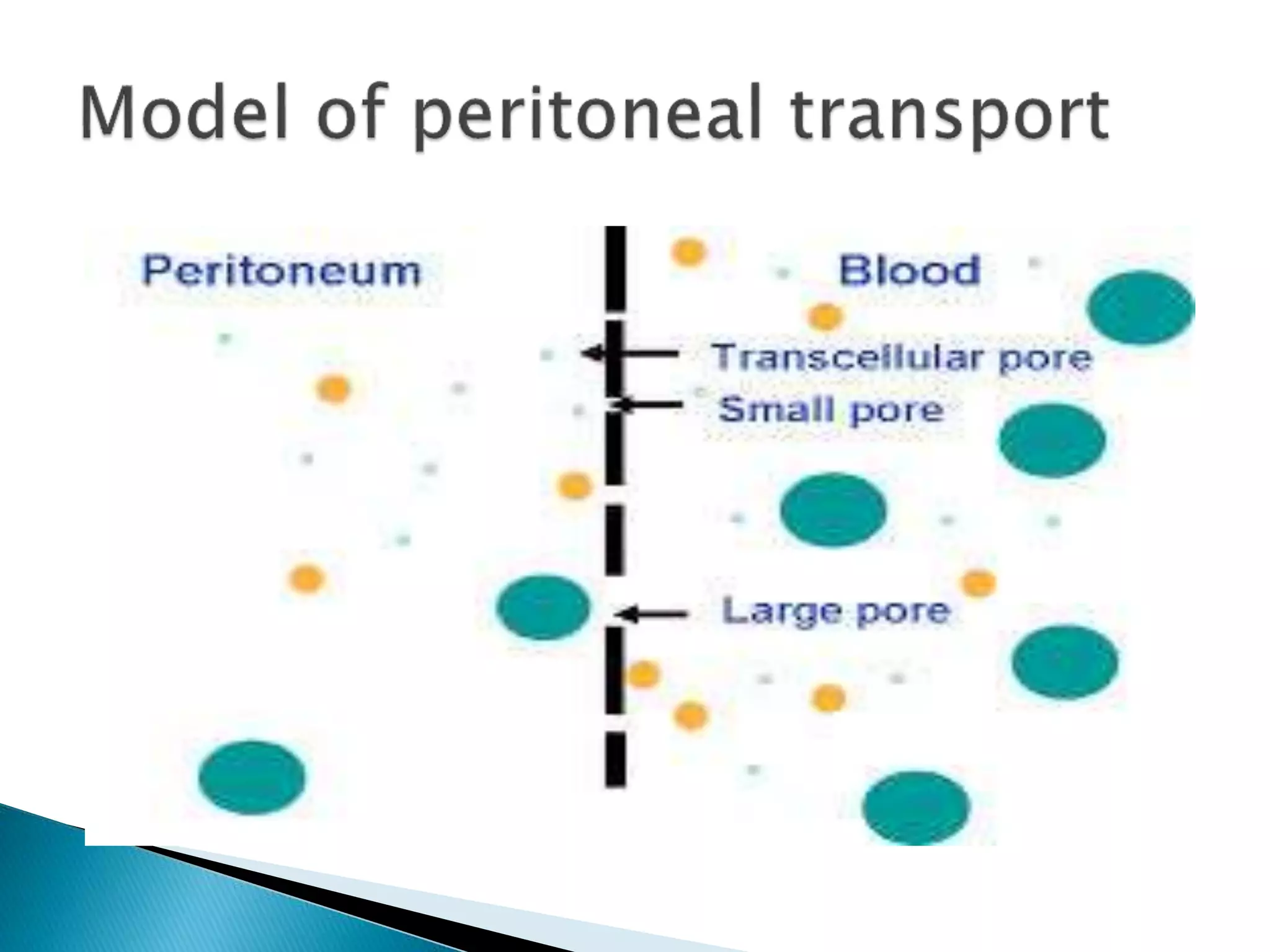
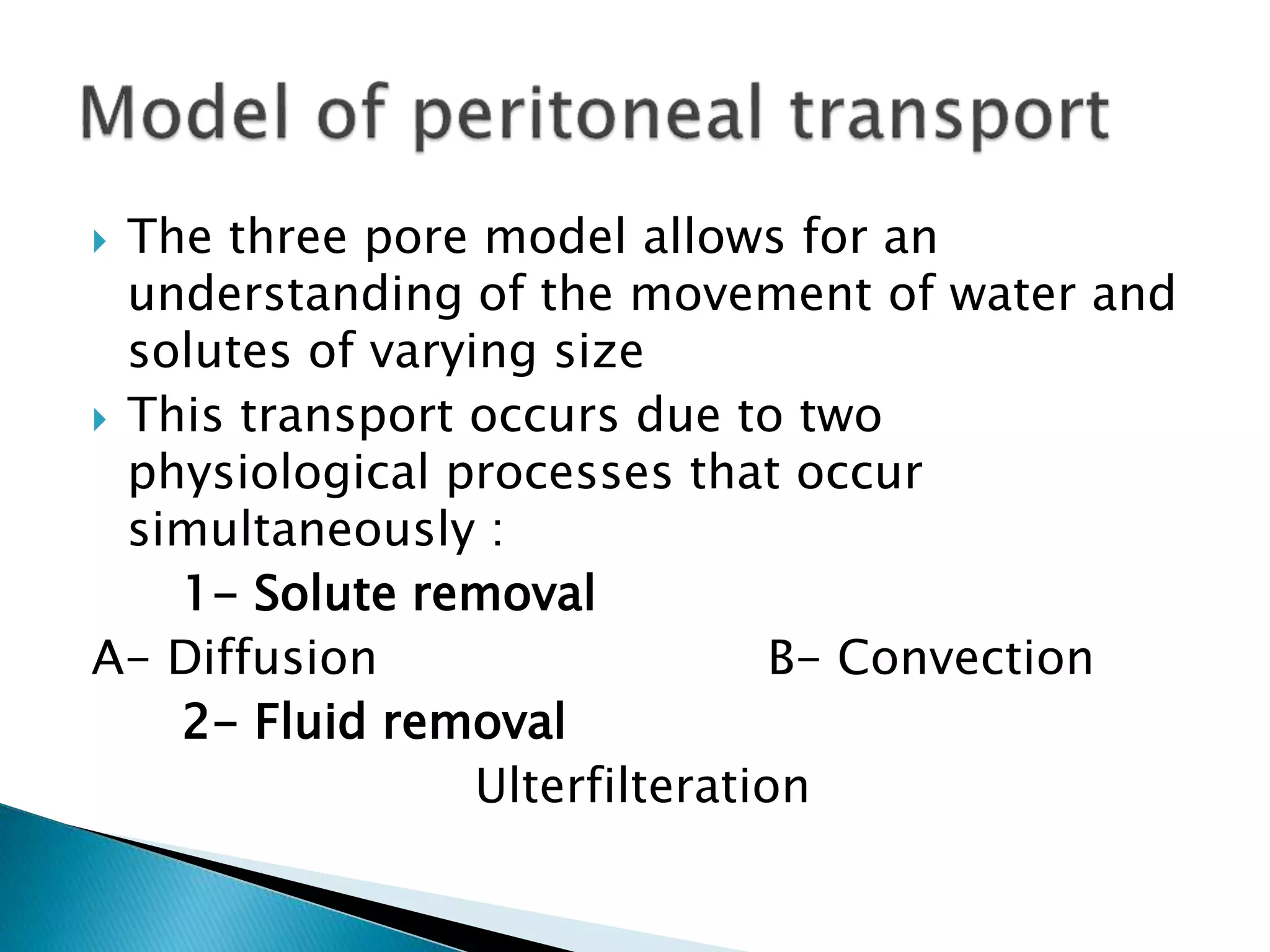
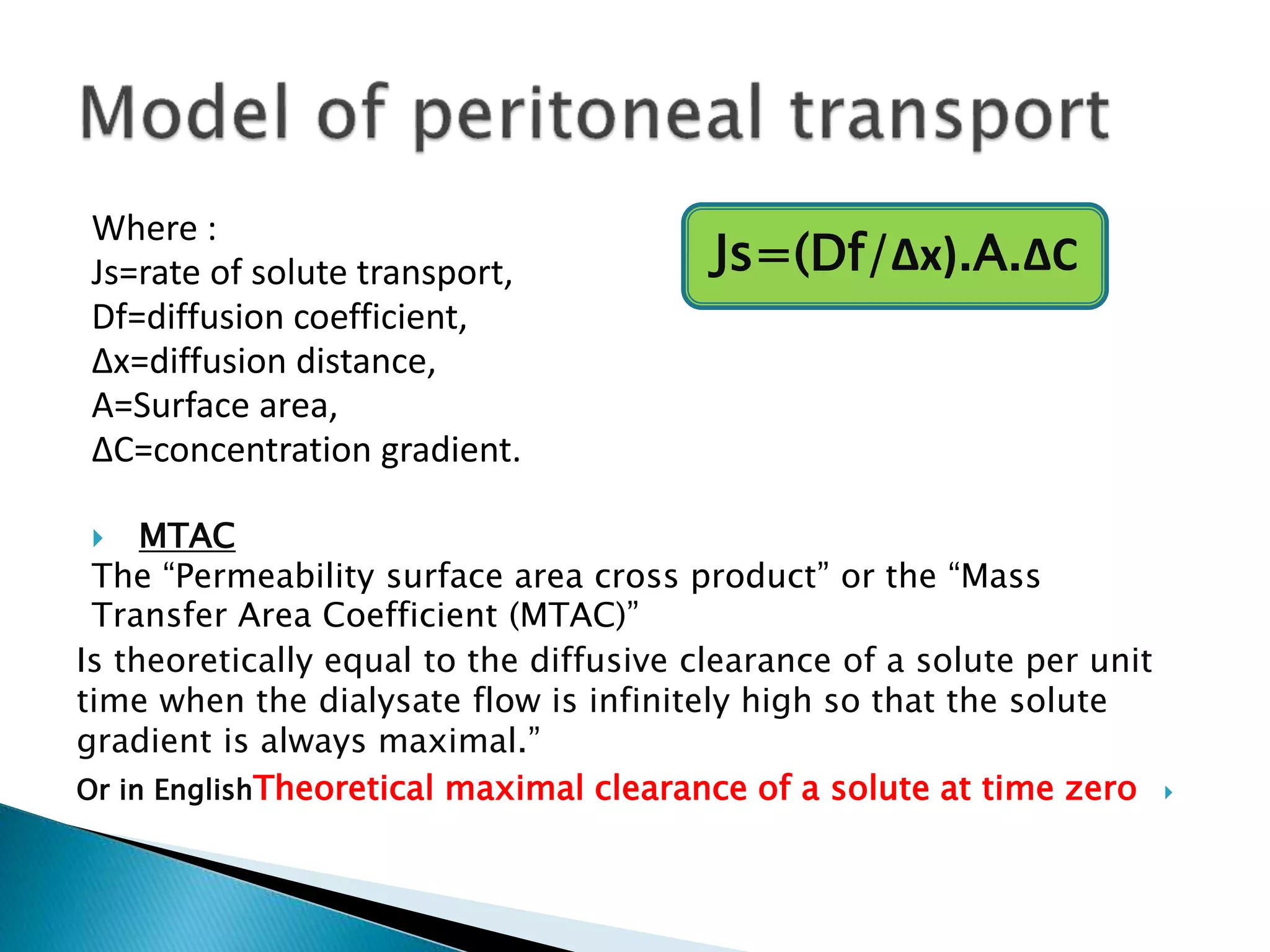
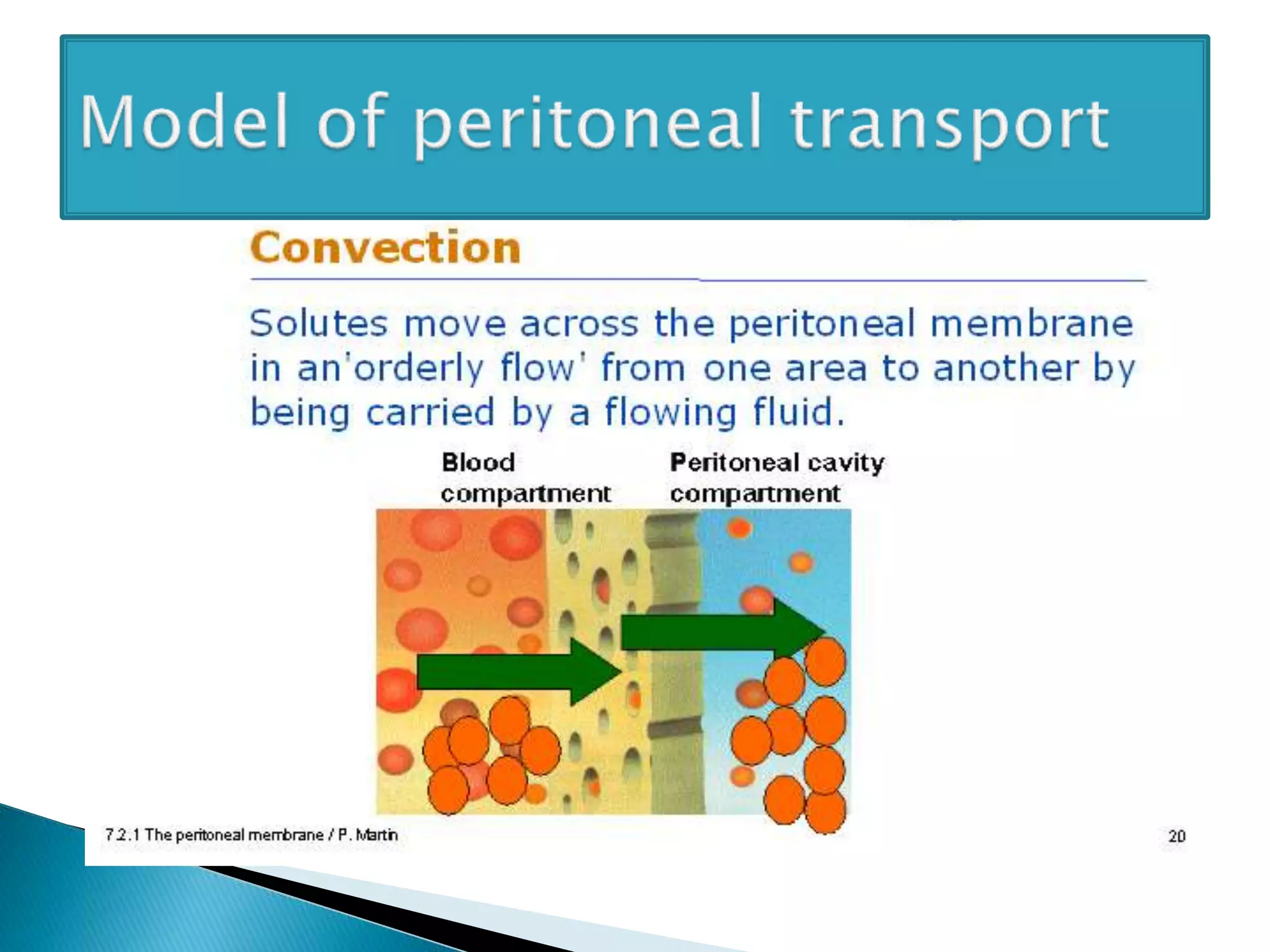
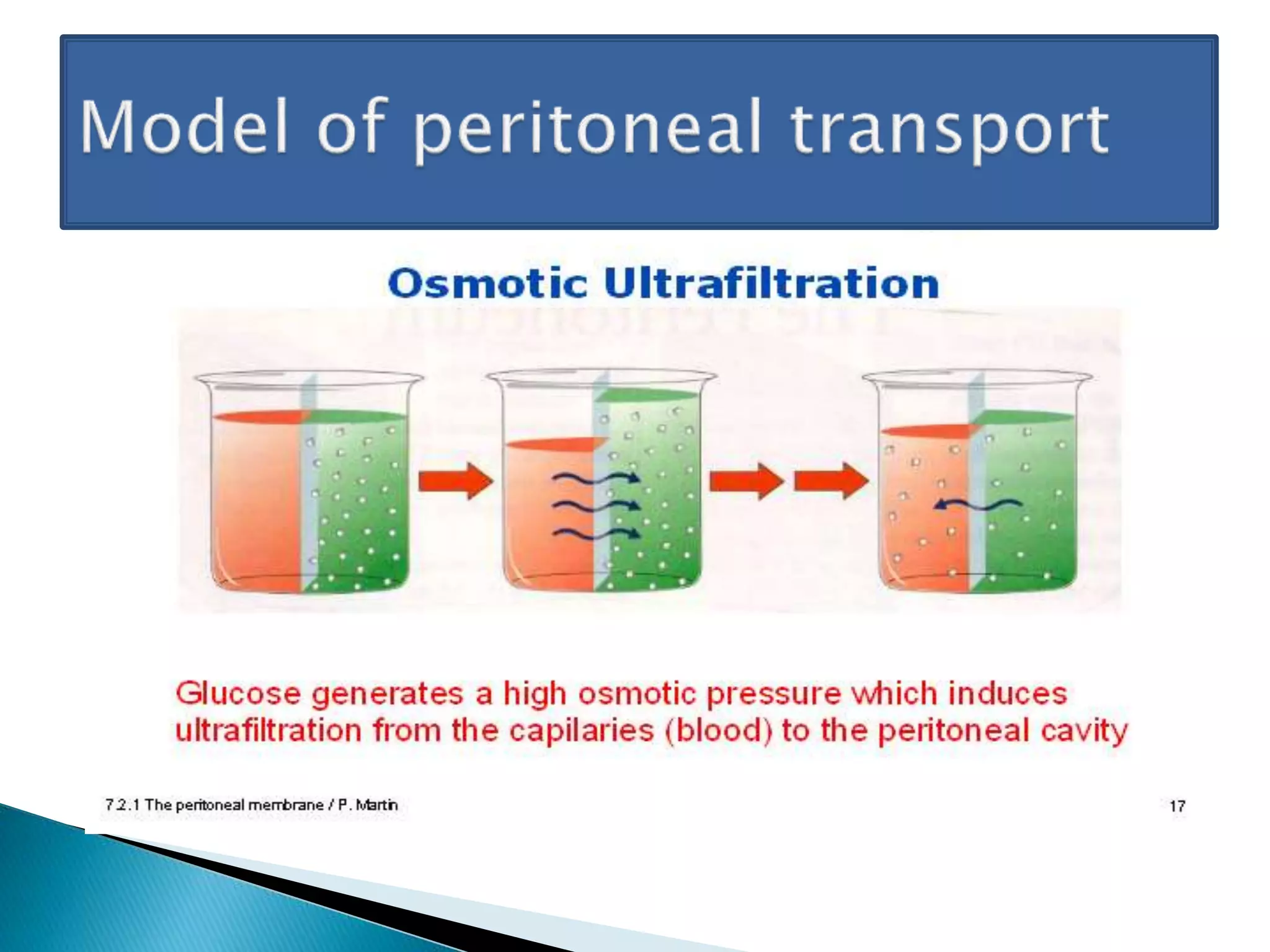
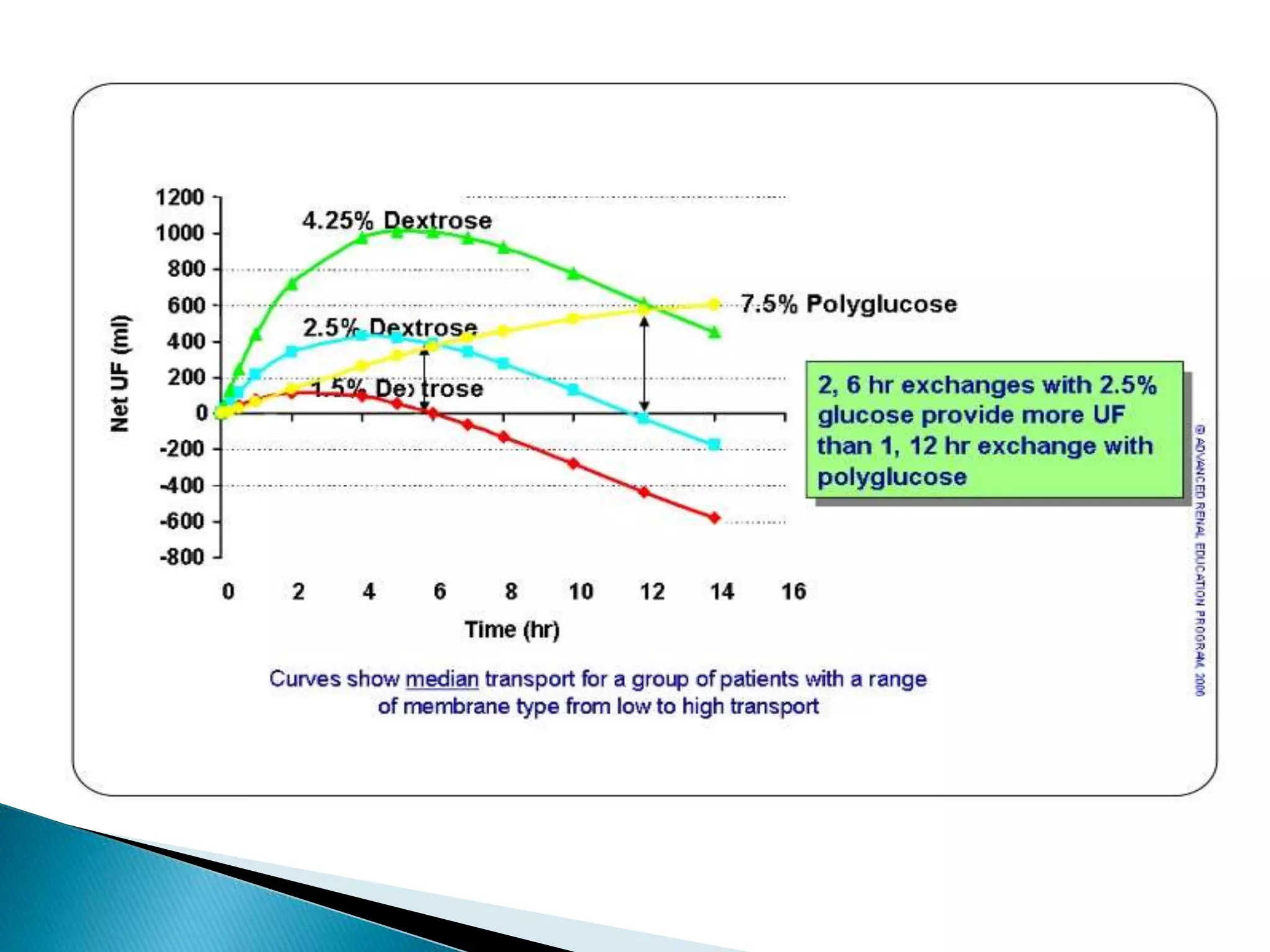
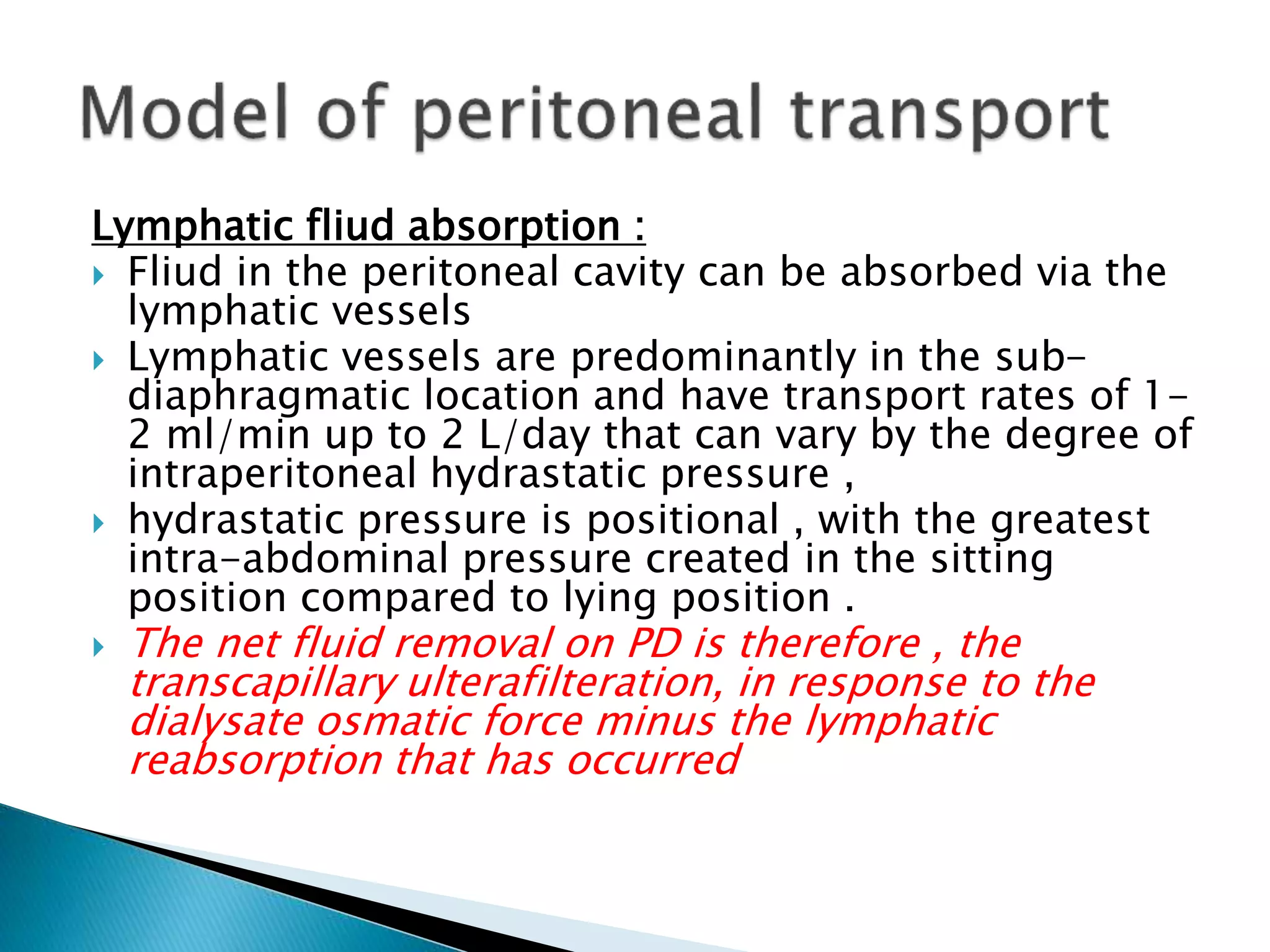
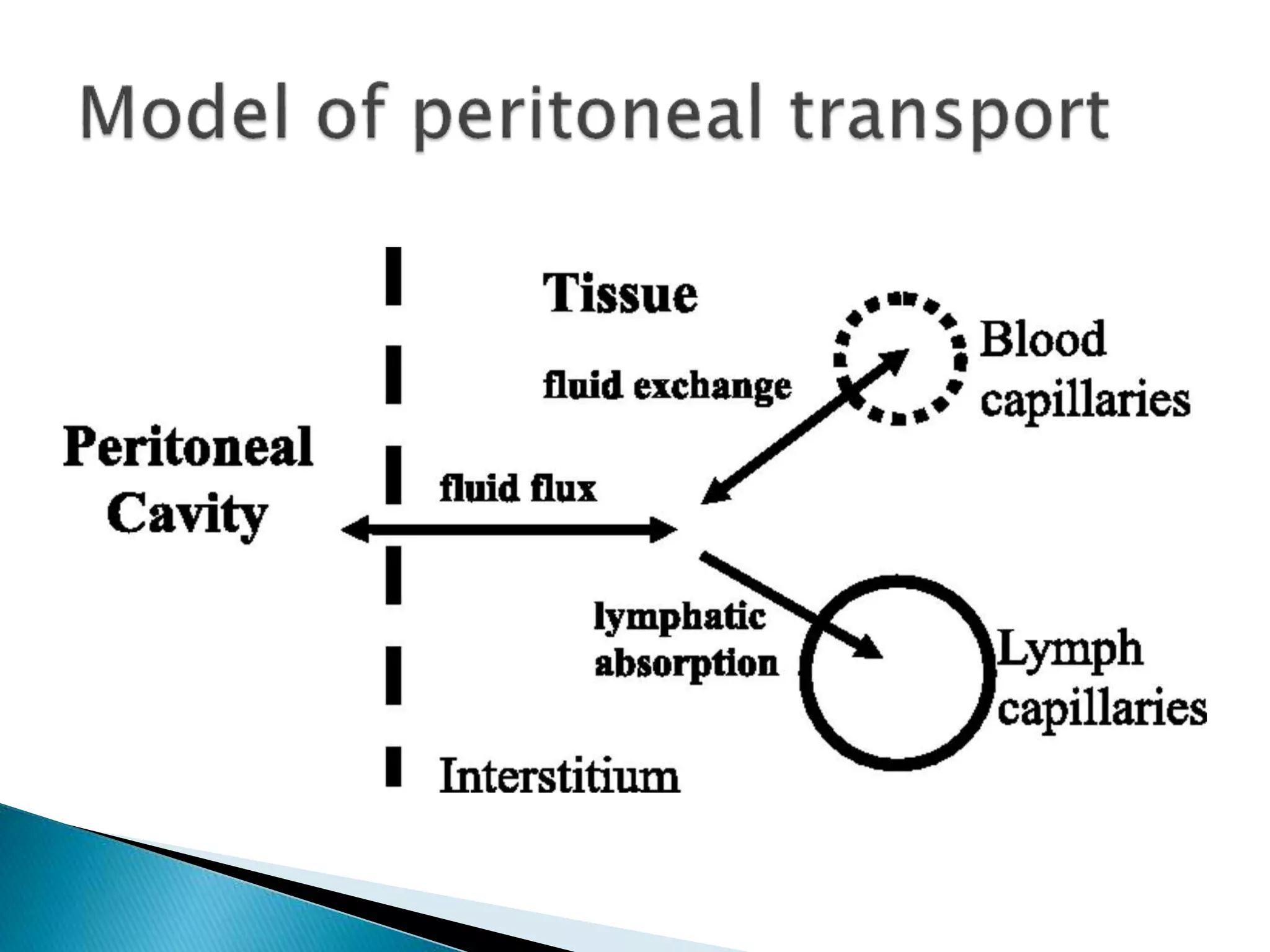
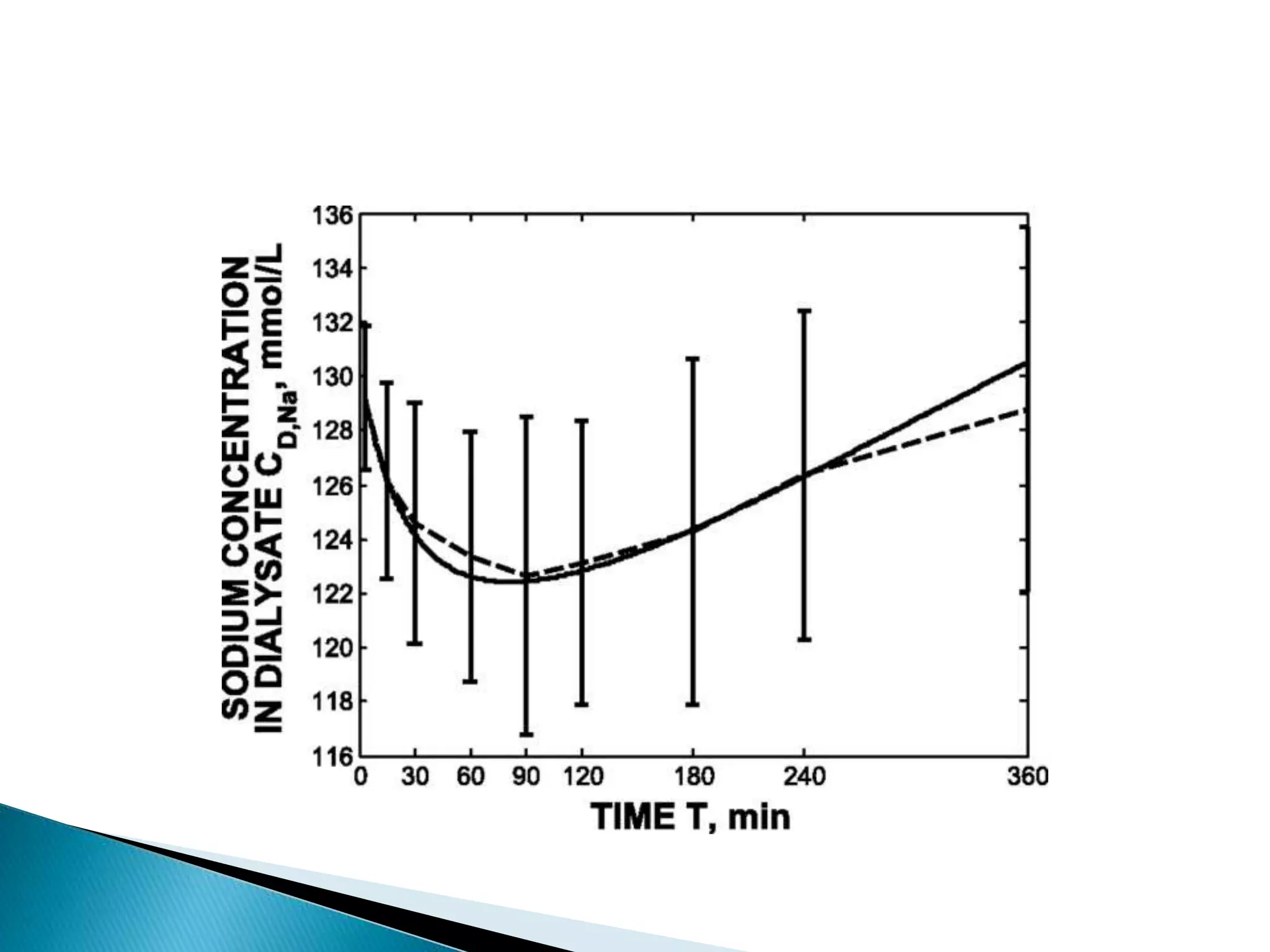
This document discusses the history and physiology of peritoneal dialysis. It outlines the key contributors to the development of PD from the 1800s onward. It then describes the anatomy of the peritoneal membrane and its blood supply. The three pore model of peritoneal transport is explained, including diffusion, convection, ultrafiltration and their roles in solute and fluid removal. Long term changes to the peritoneal membrane are also summarized.