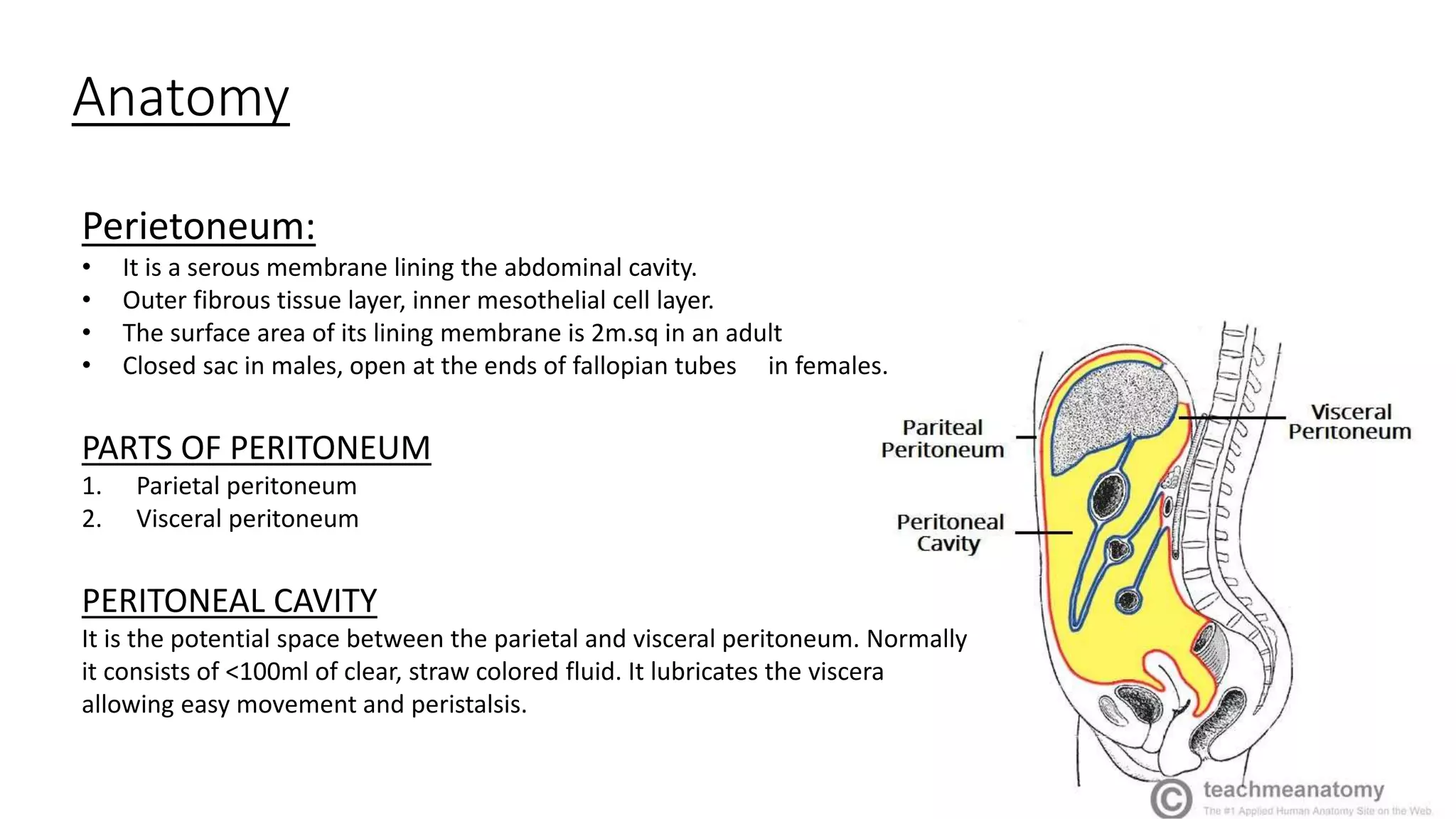
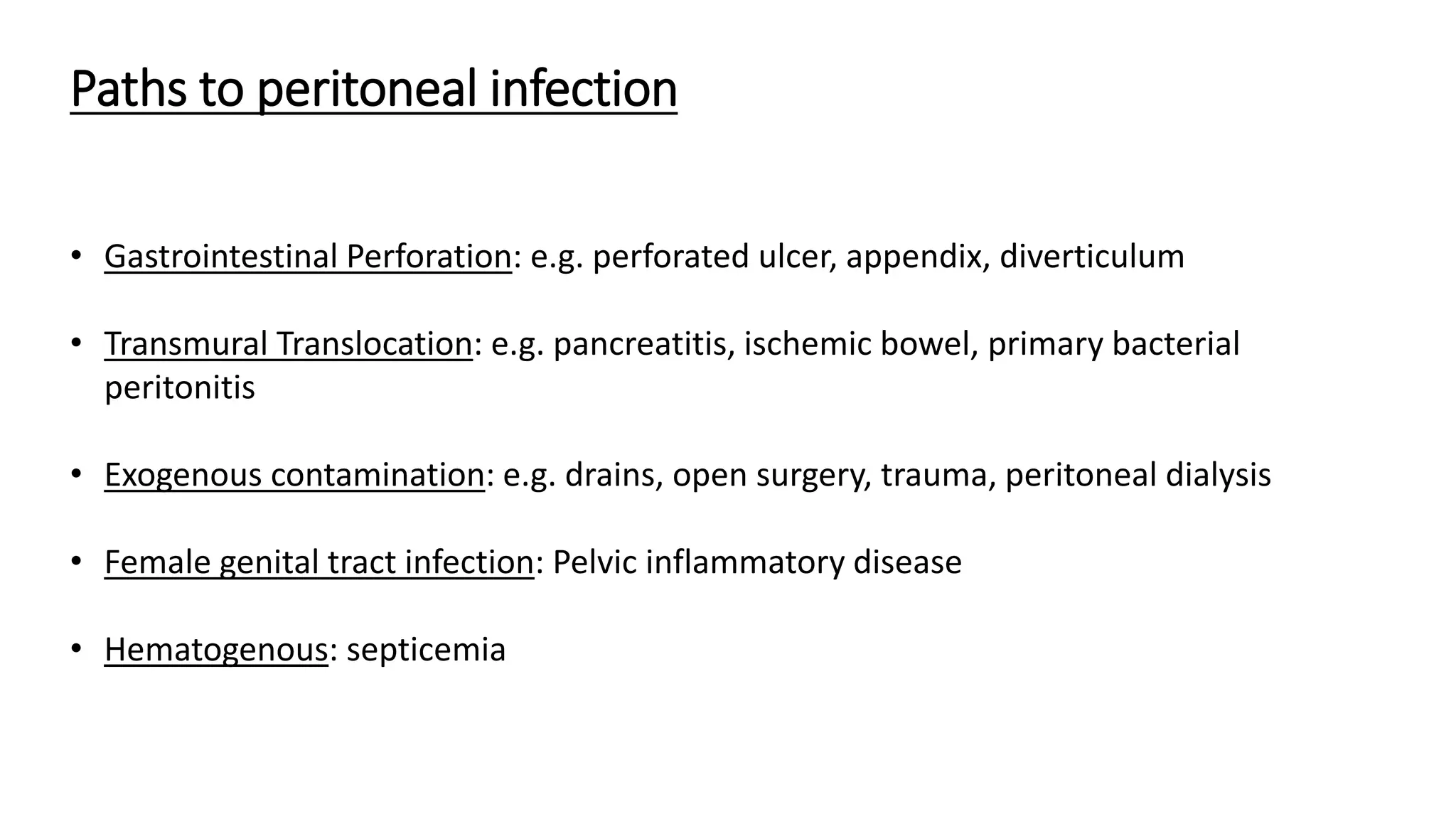
Peritonitis is inflammation of the peritoneum lining the abdominal cavity that can be caused by bacterial infection, chemicals, or trauma. The peritoneum has a parietal layer lining the abdominal wall and a visceral layer surrounding organs. Peritonitis can be primary (from spontaneous bacterial infection), secondary (from a perforated organ), or tertiary (persistent infection after treatment). Common causes are perforated ulcers or appendicitis. Patients experience abdominal pain and tenderness along with fever. Diagnosis involves blood tests and imaging scans. Treatment requires antibiotics, source control through surgery if needed, and organ support. Complications can include sepsis, multiple organ dysfunction, and death if not properly managed.