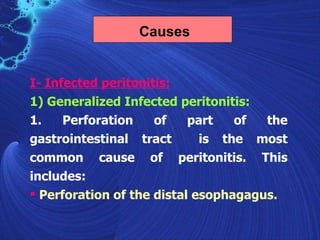
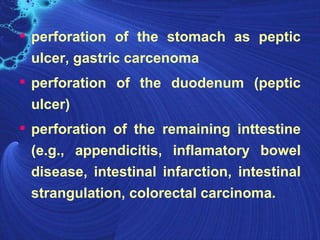
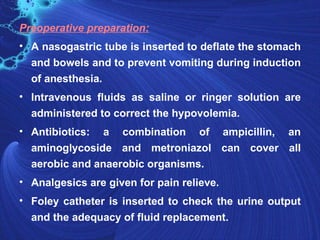
Peritonitis is an inflammation of the peritoneum that can be caused by infection or non-infectious processes. It is typically caused by a perforation or leak in the gastrointestinal tract that allows bacteria to enter the abdominal cavity. The document outlines the types, causes, signs and symptoms, diagnostic workup, and treatment including antibiotics, surgery, and postoperative care for managing peritonitis.

![[10]- Complications
Sequestration of fluid and electrolytes, as
revealed by decreased centeral venous pressure,
may cause electrolytes disturbances.
hypovolemia, leading to shock and acute renal
failure.
A peritoneal abscess.
sepsis may develop, so blood cultures should be
obtained.
The fluid may push on the diaphragm, causing
splinting and subsequent breathing difficulties.
Formation of fibrous tissue in the peritoneum
Adult respiratory distress syndrom.](https://image.slidesharecdn.com/peritonitis-120402130357-phpapp02/85/Peritonitis-30-320.jpg)