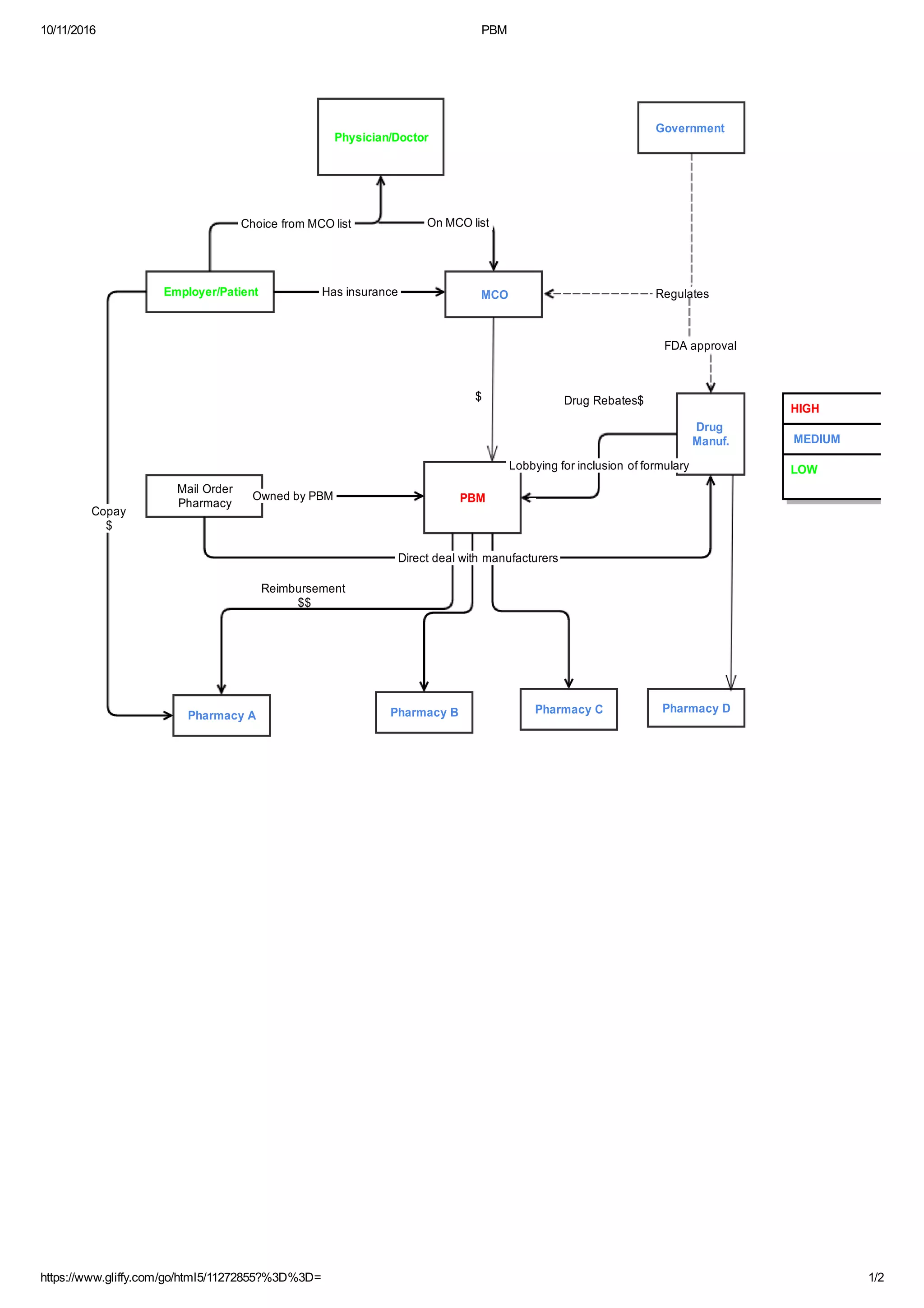
Pharmacy benefit managers (PBMs) negotiate rebates from drug manufacturers for including their drugs on formularies. PBMs own mail-order pharmacies and can make direct deals with manufacturers, earning rebates not passed to health plans or patients. PBMs are hired by health plans and employers to manage drug benefits and reimburse retail pharmacies, but also have conflicts of interest due to rebates and mail-order ownership. Government regulates drug approval through the FDA but not PBM business practices that can impact costs for employers, health plans, and patients.