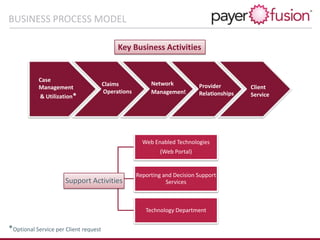
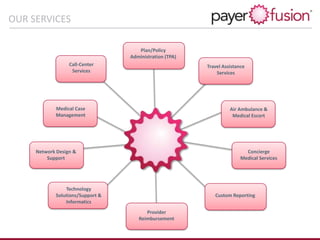
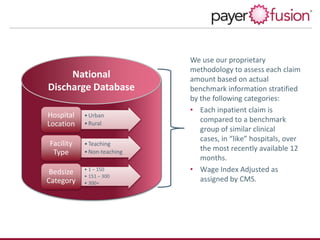
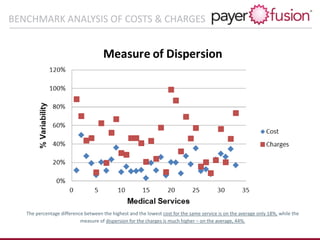
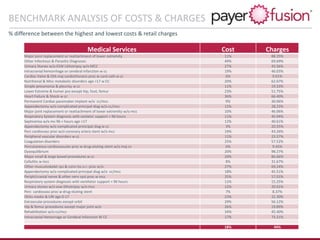
PayerFusion is a Six Sigma-focused company providing next-generation claims management and cost containment solutions for insurance companies and providers, utilizing HIPAA-compliant technology. Their services include a proprietary provider network, custom software, and expertise in billing guidelines, aimed at reducing claim payment cycles and administrative costs while promoting client branding. Founded in 2009 and backed by a seasoned management team, PayerFusion operates with licenses across all states, ensuring compliance and integrity in their operations.