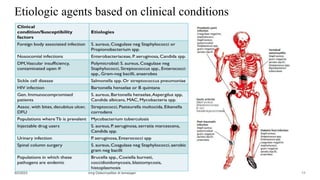
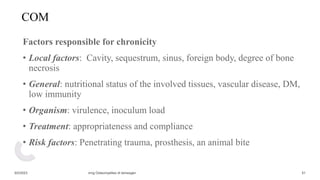
This document provides an overview of the management of osteomyelitis. It begins by defining osteomyelitis as a suppurative bone infection caused by pyogenic organisms. It then covers the classification, etiology, pathogenesis, clinical presentation, diagnosis and treatment of both acute and chronic osteomyelitis. For acute osteomyelitis, the document highlights hematogenous spread as the main mechanism and emphasizes the importance of Staphylococcus aureus. It also outlines the pathophysiology, presentations, investigations and management including antibiotics and possible surgery. For chronic osteomyelitis, it discusses predisposing factors, classification systems, surgical debridement approaches and the goals of long-term treatment and limb salvage.