Occupational radiation safety in Radiological imaging
1) There is increased use of radiation-based medical imaging globally, but many staff lack proper training in radiation safety techniques.
2) Workers in cardiology cath labs receive the highest radiation doses, followed by radiology cath labs and other interventional procedures. Prolonged fluoroscopic screening can lead to hair loss and cataracts in interventionalists.
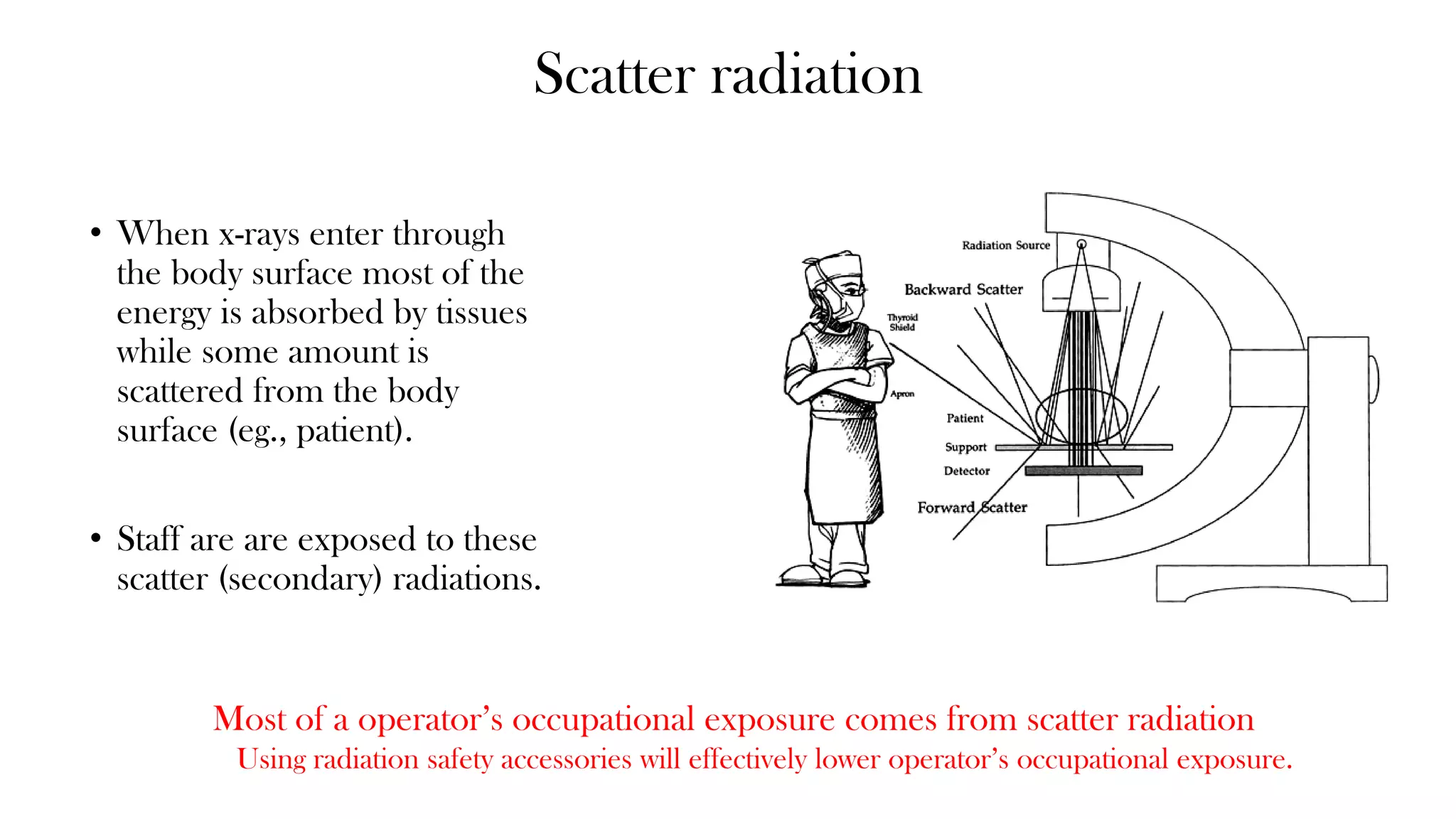
3) Basic principles of radiation safety include minimizing time, maximizing distance, and using shielding. Monitoring staff doses with dosimeters and following safety protocols helps ensure doses are as low as reasonably achievable.