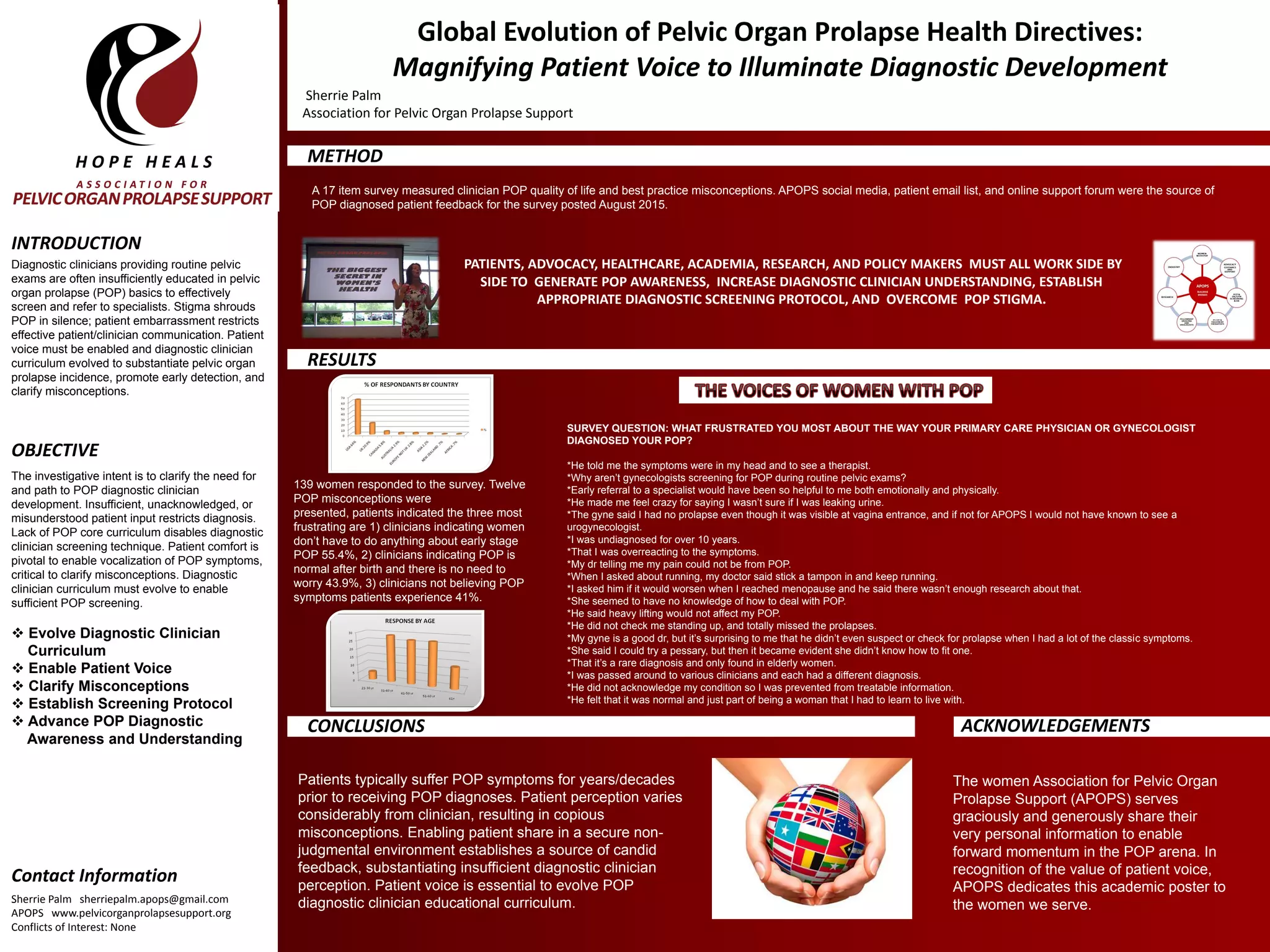
This document discusses the need to improve diagnostic clinician education about pelvic organ prolapse (POP) by incorporating patient experiences and perspectives. A survey of 139 POP patients found common misconceptions among clinicians that minimized or dismissed POP symptoms. Examples of frustrating patient experiences show clinicians often lacked knowledge to properly diagnose or treat POP. The conclusion is that patient input is essential to evolve diagnostic clinician curriculum and address insufficient perceptions about POP. Enabling patient voices can help establish appropriate screening protocols and awareness of this under-recognized condition.