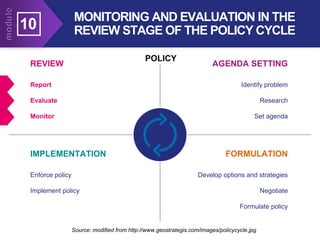
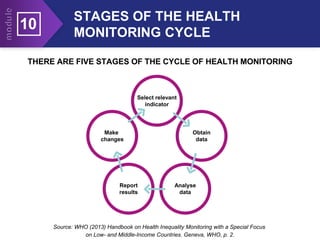
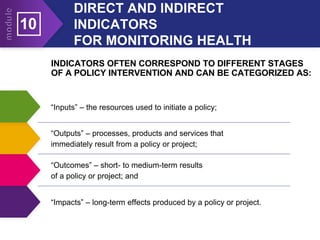
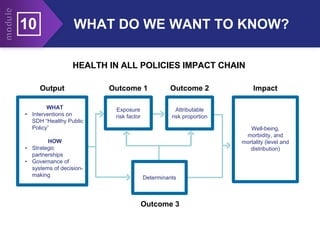
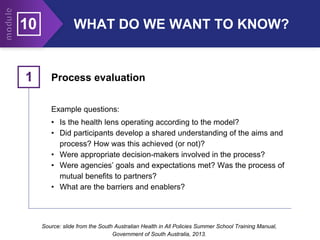
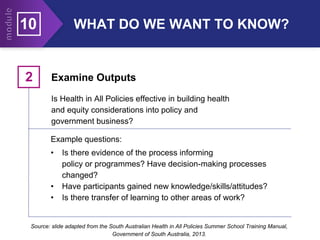
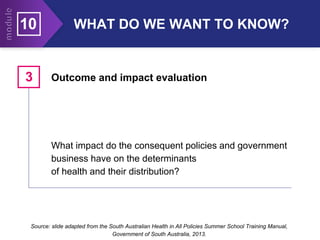
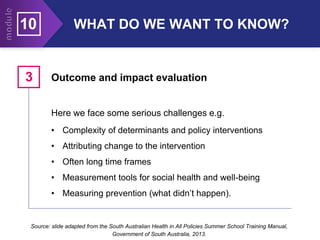
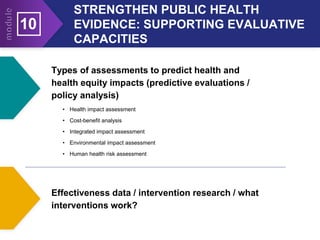
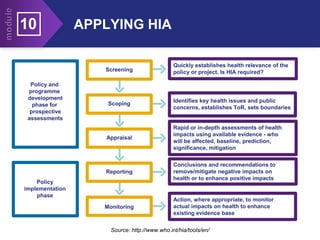
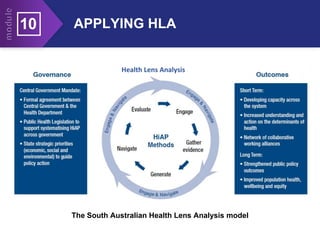
This document provides an overview of monitoring and evaluation as it relates to health policies and programs. It discusses reasons for monitoring and evaluation, different types of monitoring including inputs, outputs, outcomes and impact. It also explains the purpose and key steps of health impact assessment and health lens analysis. Sources of health data and policy advice are identified. The benefits of monitoring and evaluation are outlined including accountability, testing predictions, adding to evidence, and empowering communities. Stages of the health monitoring cycle and examples of direct and indirect indicators are provided.