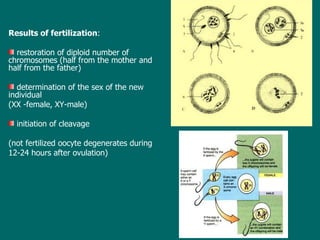
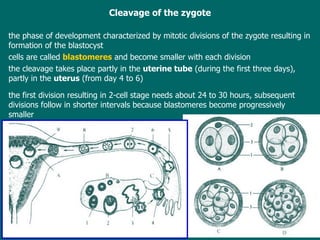
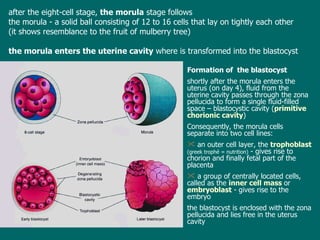
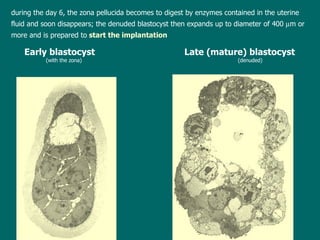
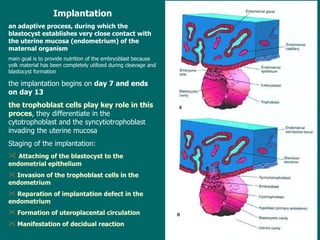
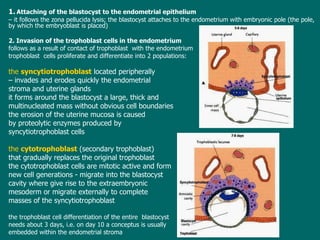
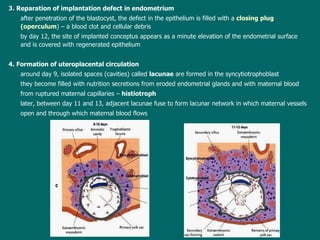
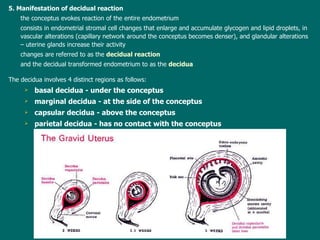
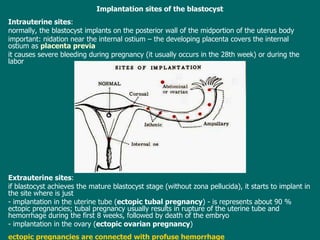
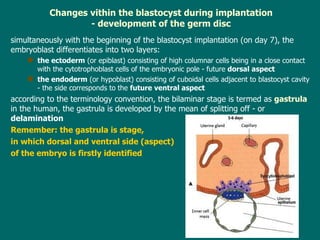
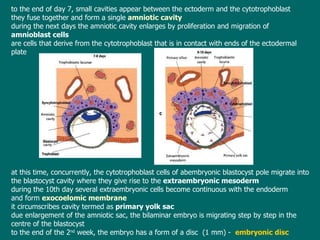
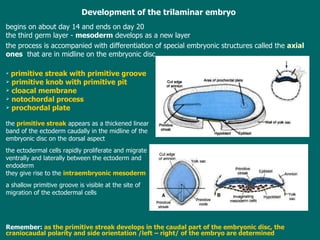
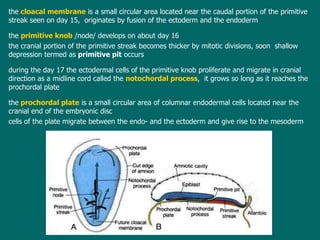
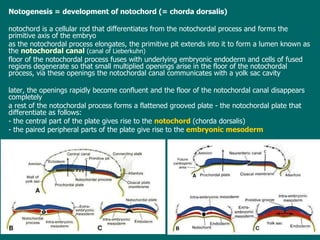
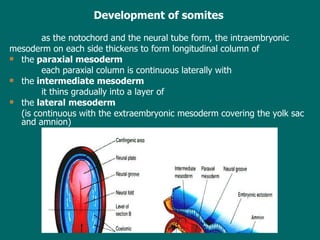
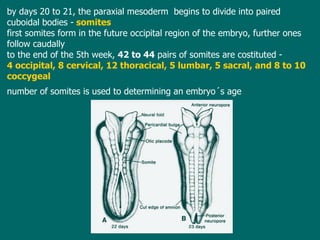
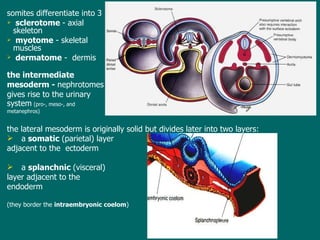
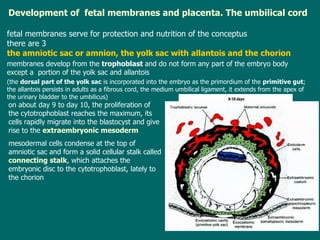
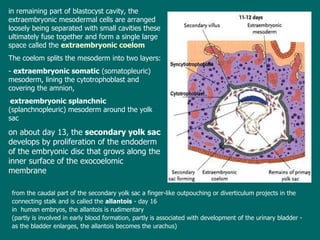
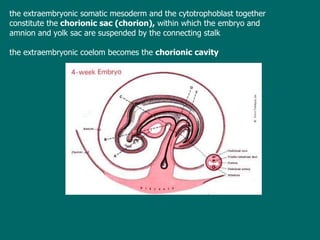
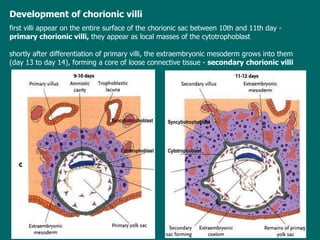
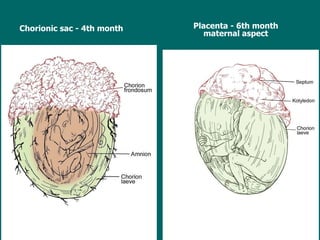
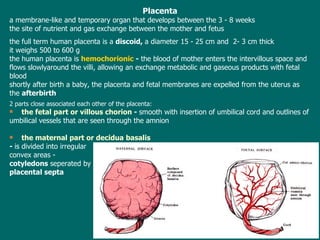
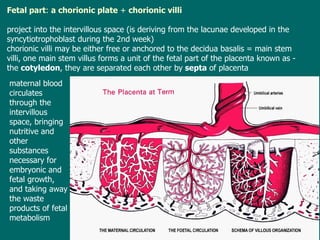
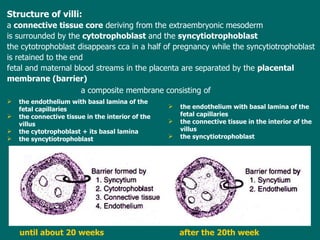
The document summarizes key stages of early human embryonic development, including implantation of the blastocyst, formation of the germ layers and germ disc, development of structures like the notochord and somites, and formation of the fetal membranes and placenta. It describes how the blastocyst attaches and invades the uterine wall during implantation between days 7-13, and how the germ layers of ectoderm, endoderm and mesoderm form by day 14, establishing the basic body plan of the embryo.