The document discusses several topics related to human reproductive cycles:
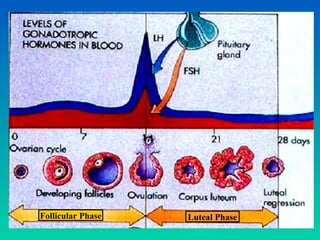
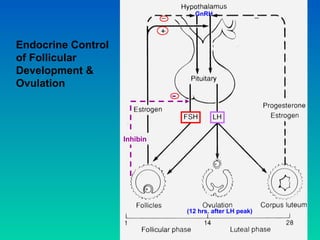
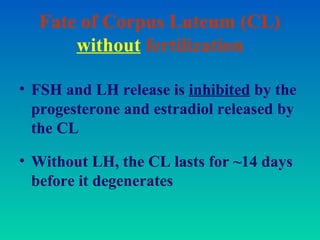
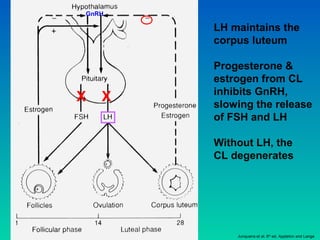
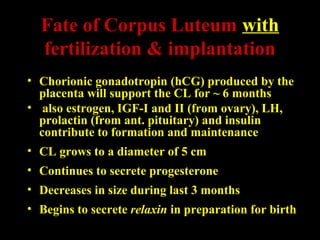
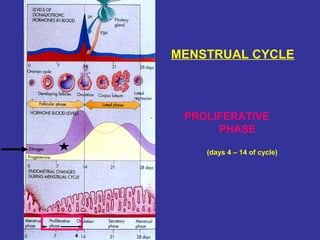
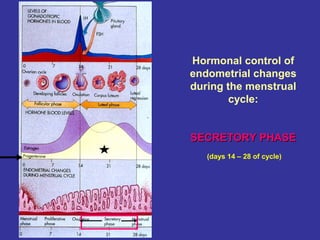
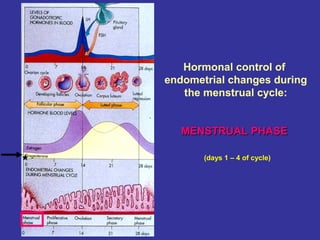
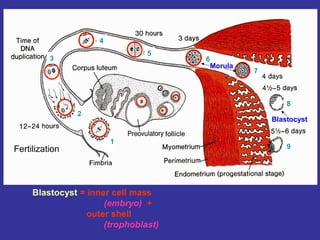
1. The ovarian cycle consists of the follicular and luteal phases, culminating in ovulation in the middle. The corpus luteum forms during the luteal phase and secretes hormones to prepare the uterus.
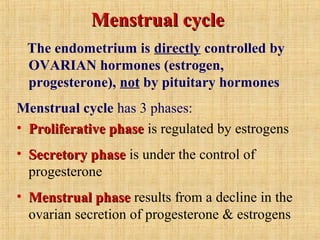
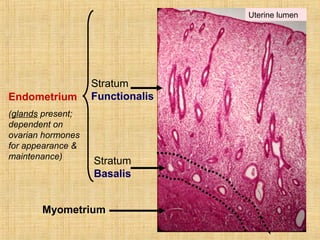
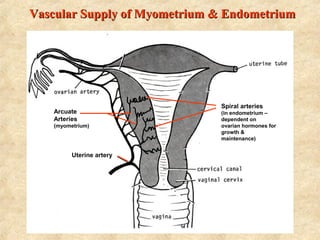
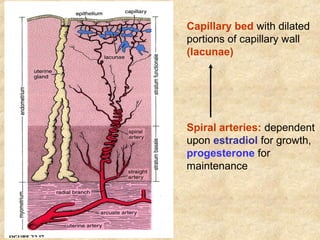
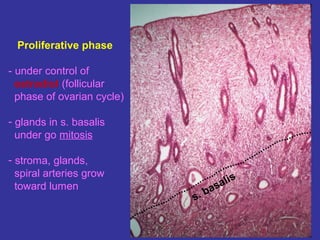
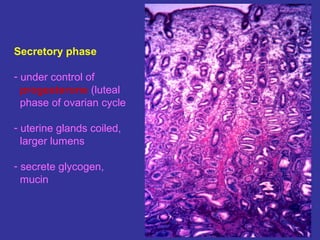
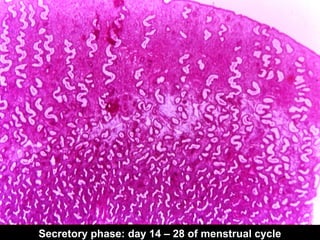
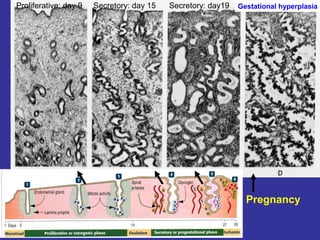
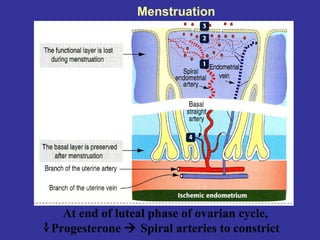
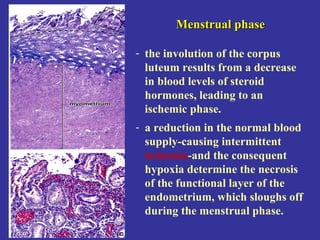
2. The menstrual cycle is controlled by ovarian hormones and has proliferative, secretory, and menstrual phases that regulate the endometrium.
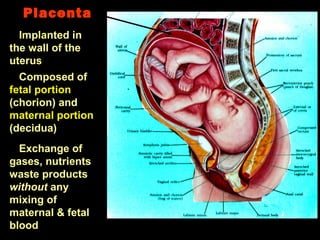
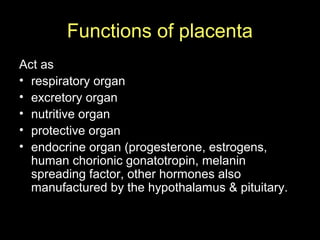
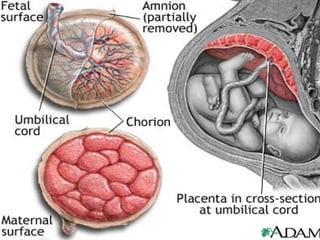
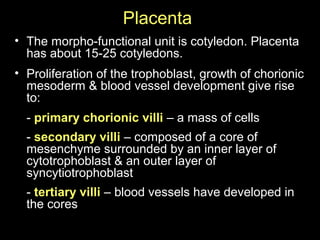
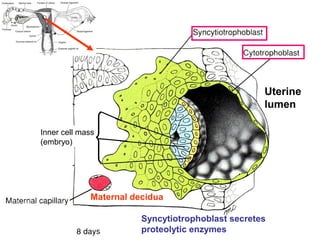
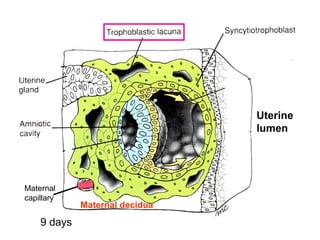
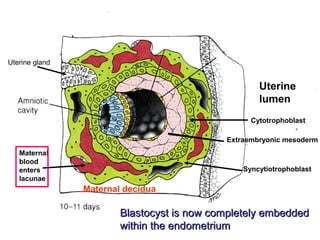
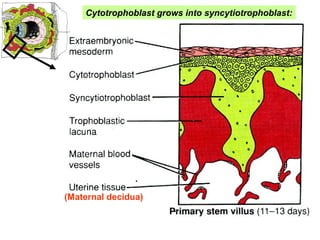
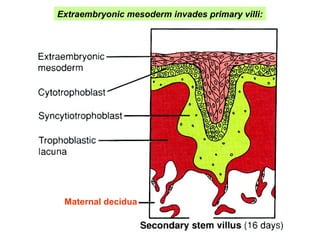
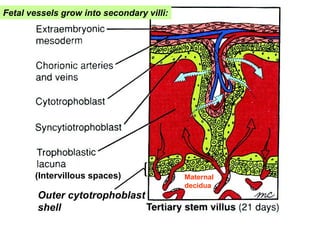
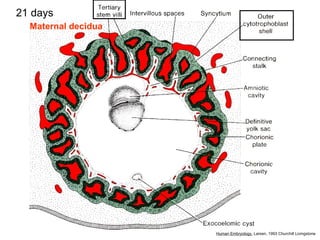
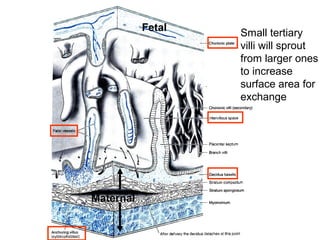
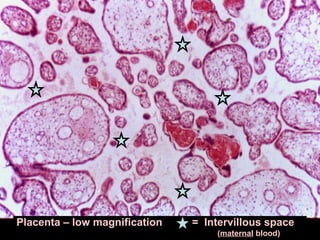
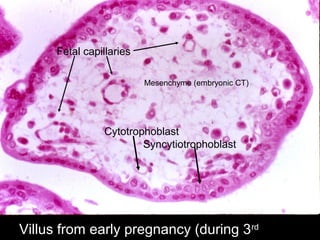
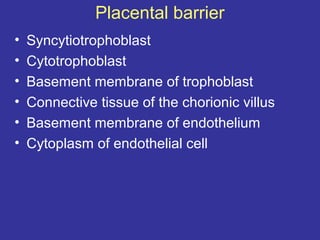
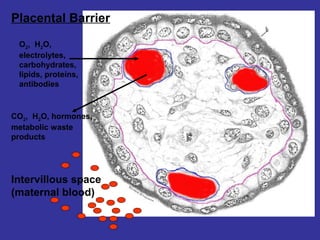
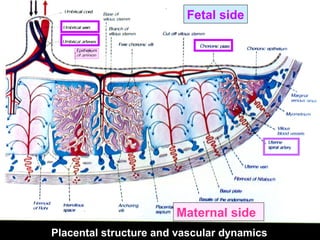
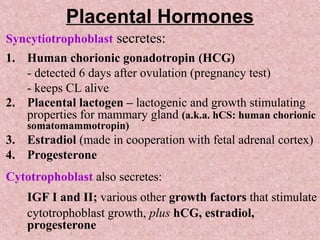
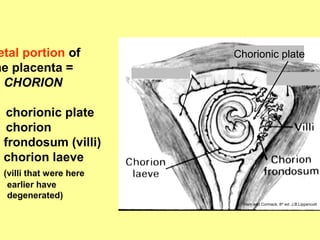
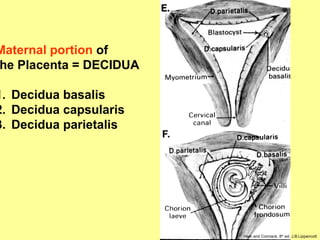
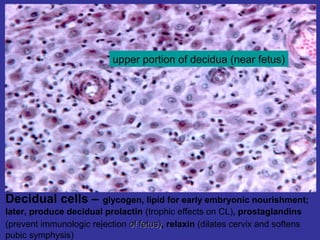
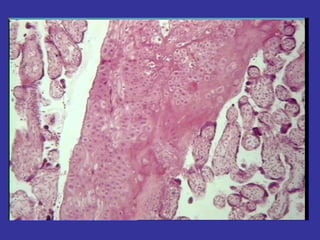
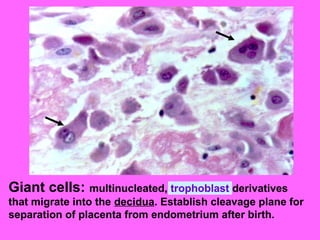
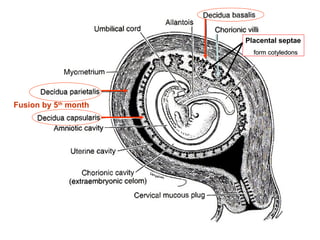
3. Placentation begins with implantation and involves the formation of chorionic villi from the embryo and decidua from the endometrium to facilitate nutrient/waste exchange between mother and fetus without blood mixing. The placenta secretes important hormones throughout pregnancy.