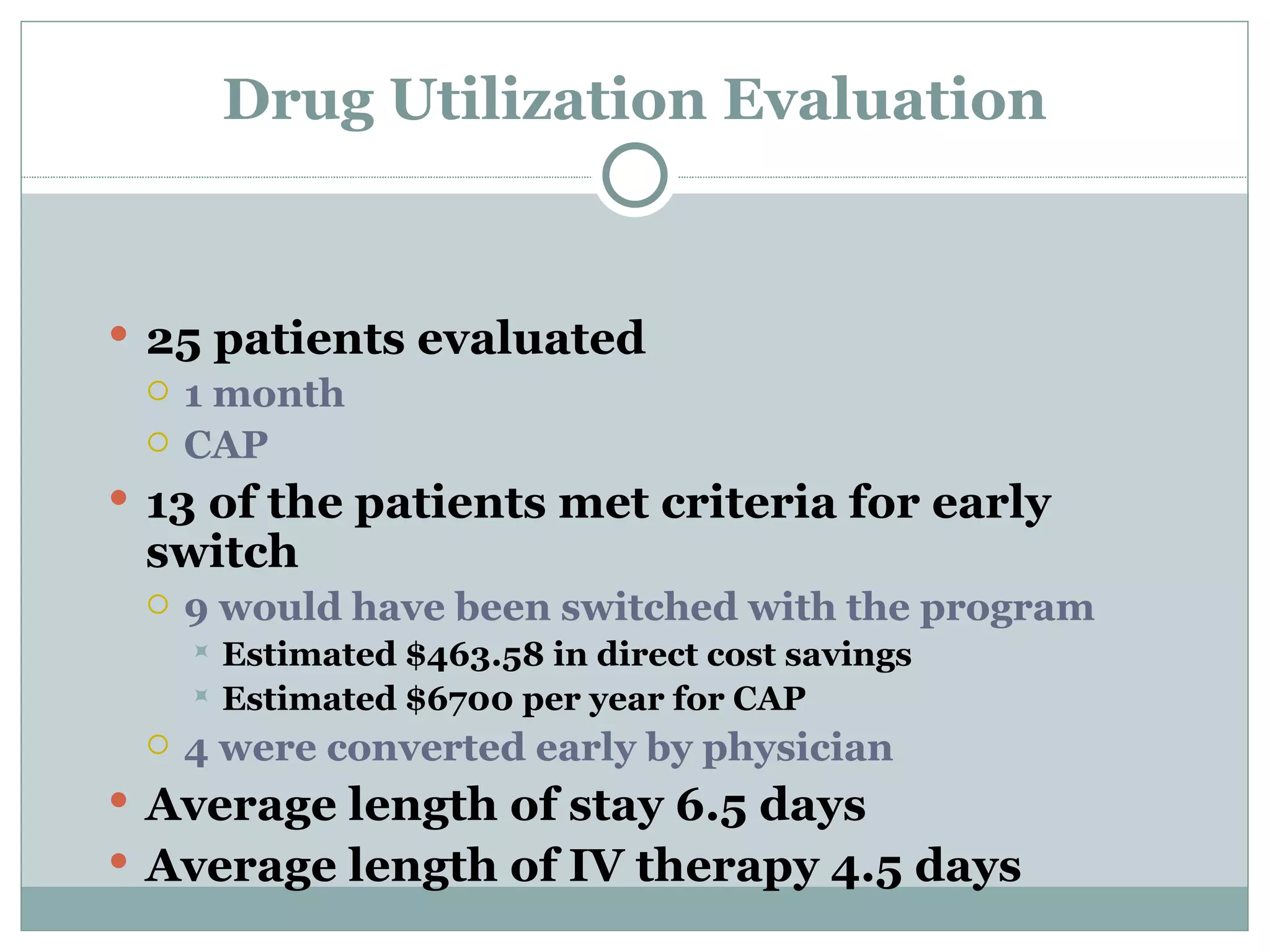
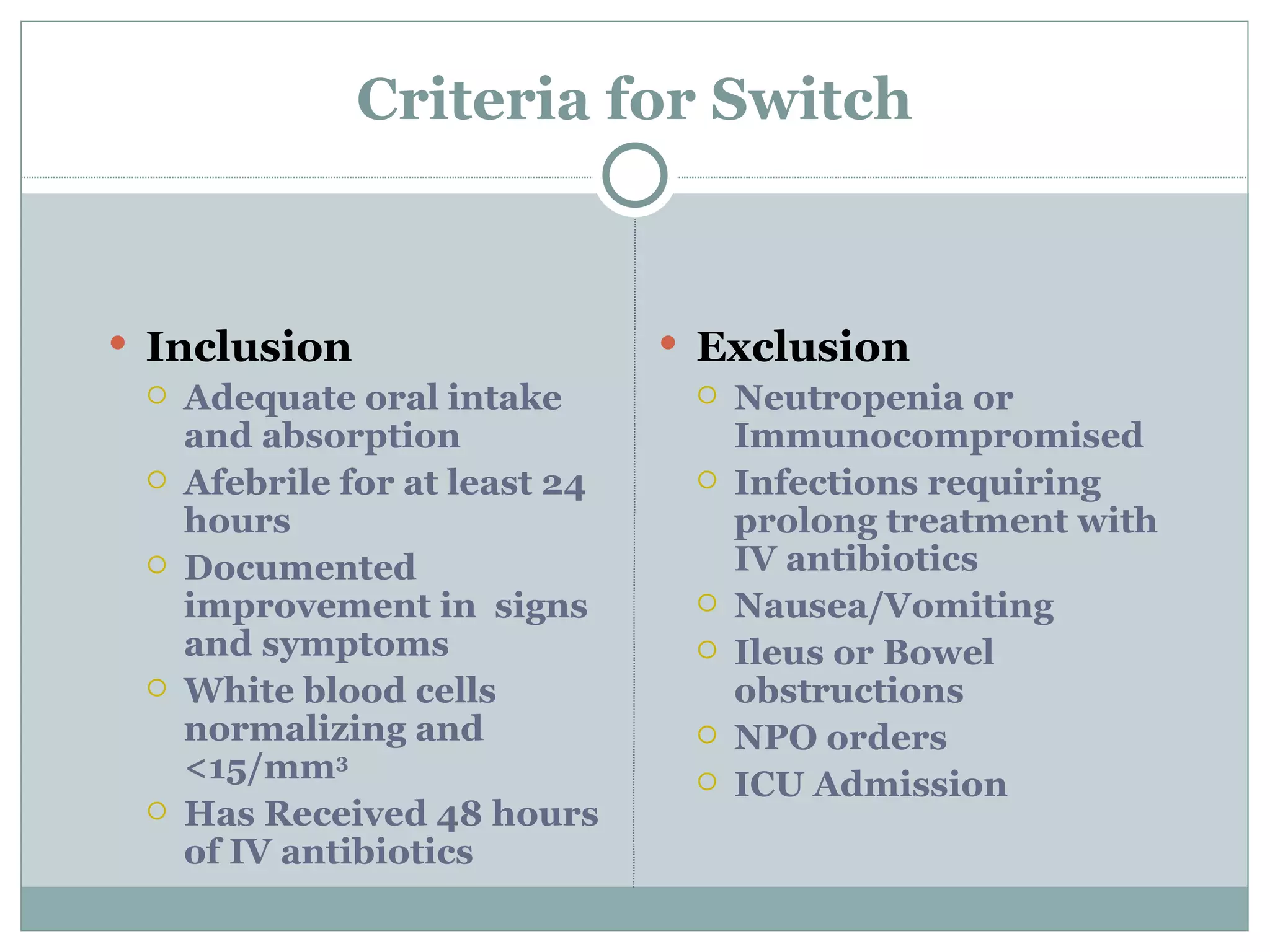
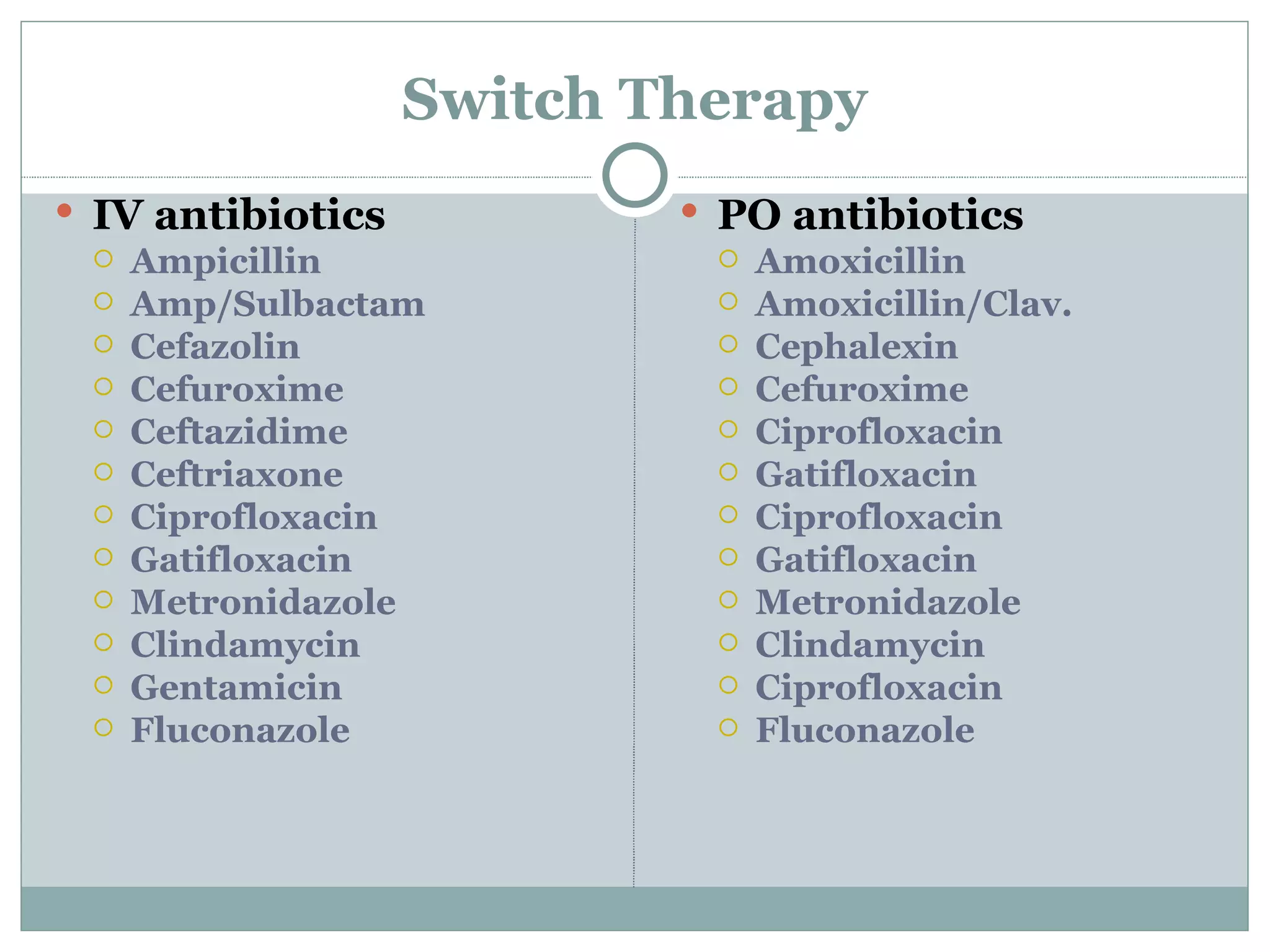
Ryan Mills, a pharmacist candidate, evaluated implementing a program at Charleston Area Medical Center to switch patients earlier from intravenous to oral antibiotics based on certain criteria. In a study of 25 patients with community-acquired pneumonia, 13 met criteria for early switch, which could have resulted in over $400 in direct cost savings annually. The goals of the program were to maintain or improve outcomes while decreasing costs of IV drugs and patient care. A follow-up evaluation of 30% of patients switched found 100% cure rates with average cost savings of $44 per patient and decreased length of IV therapy.