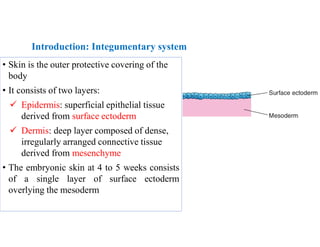
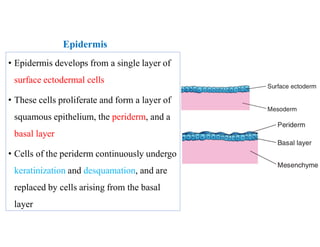
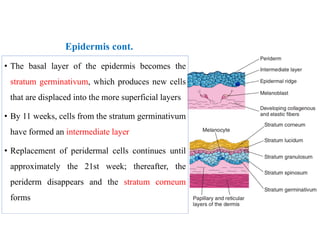
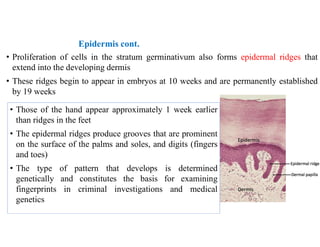
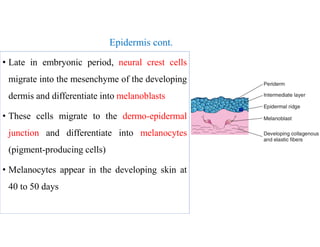
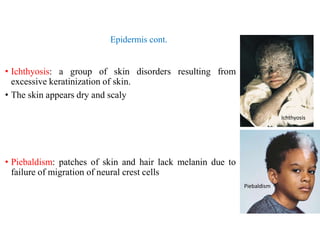
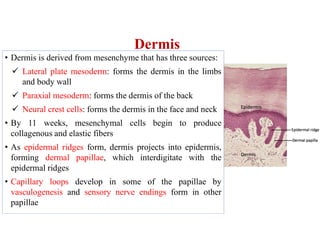
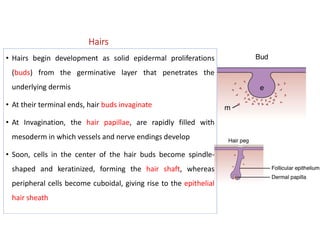
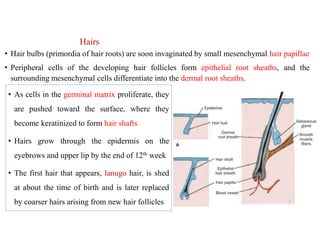
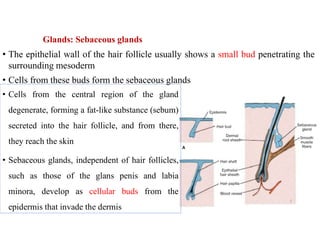
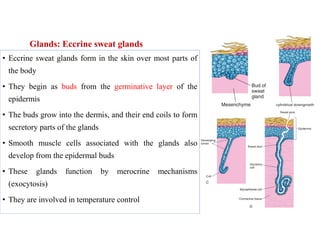
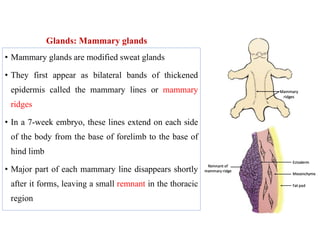
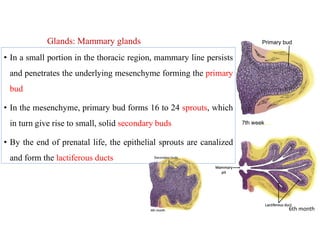
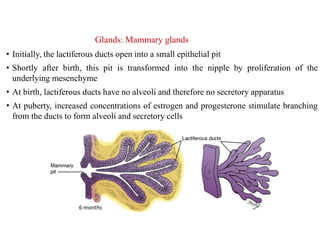
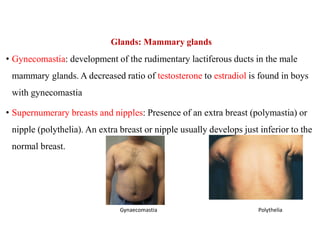
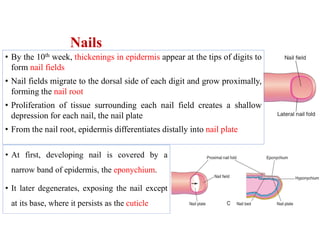
This document provides information about a lecture on the development of the integumentary system that will take place on December 5th, 2022. It discusses the objectives of describing skin, gland, and nail development and identifying congenital malformations. It then summarizes the development of the epidermis, dermis, hair, sebaceous glands, sweat glands, mammary glands, and nails. It also briefly describes several congenital disorders that can affect the integumentary system, such as ichthyosis, piebaldism, gynecomastia, and aplastic anonychia. The document concludes by noting that the next lecture will cover skeletal system development and instructing students