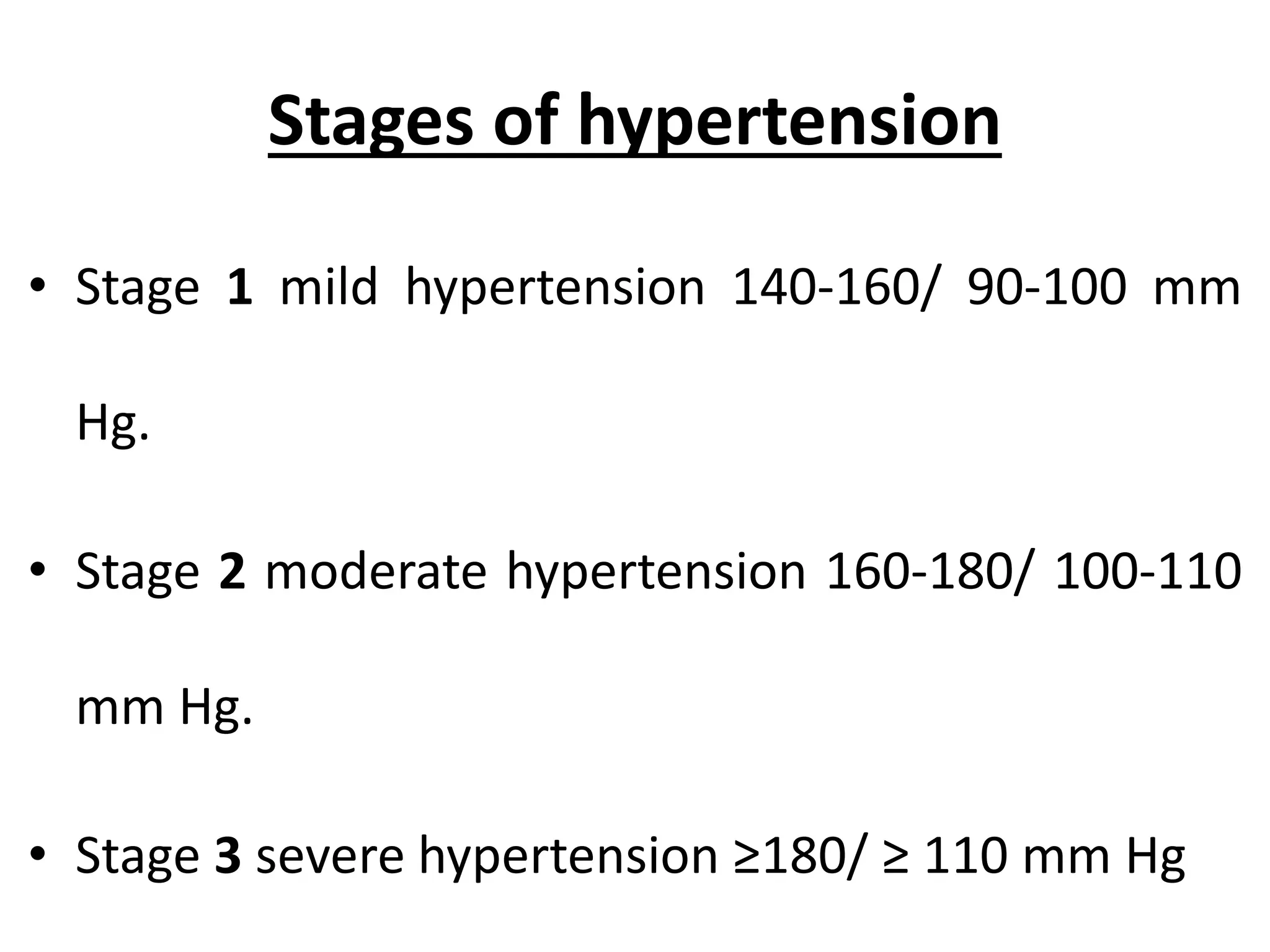
Hypertension, also known as high blood pressure, is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. It is defined as a systolic pressure above 140 mmHg or a diastolic pressure above 90 mmHg. Hypertension has stages from mild to severe and usually does not cause symptoms, but long-term can lead to serious health issues like heart disease or stroke if not managed. Risk factors include age, family history, obesity, smoking, diet high in salt, and lack of exercise. Treatment involves lifestyle changes and medications to control blood pressure and prevent complications.