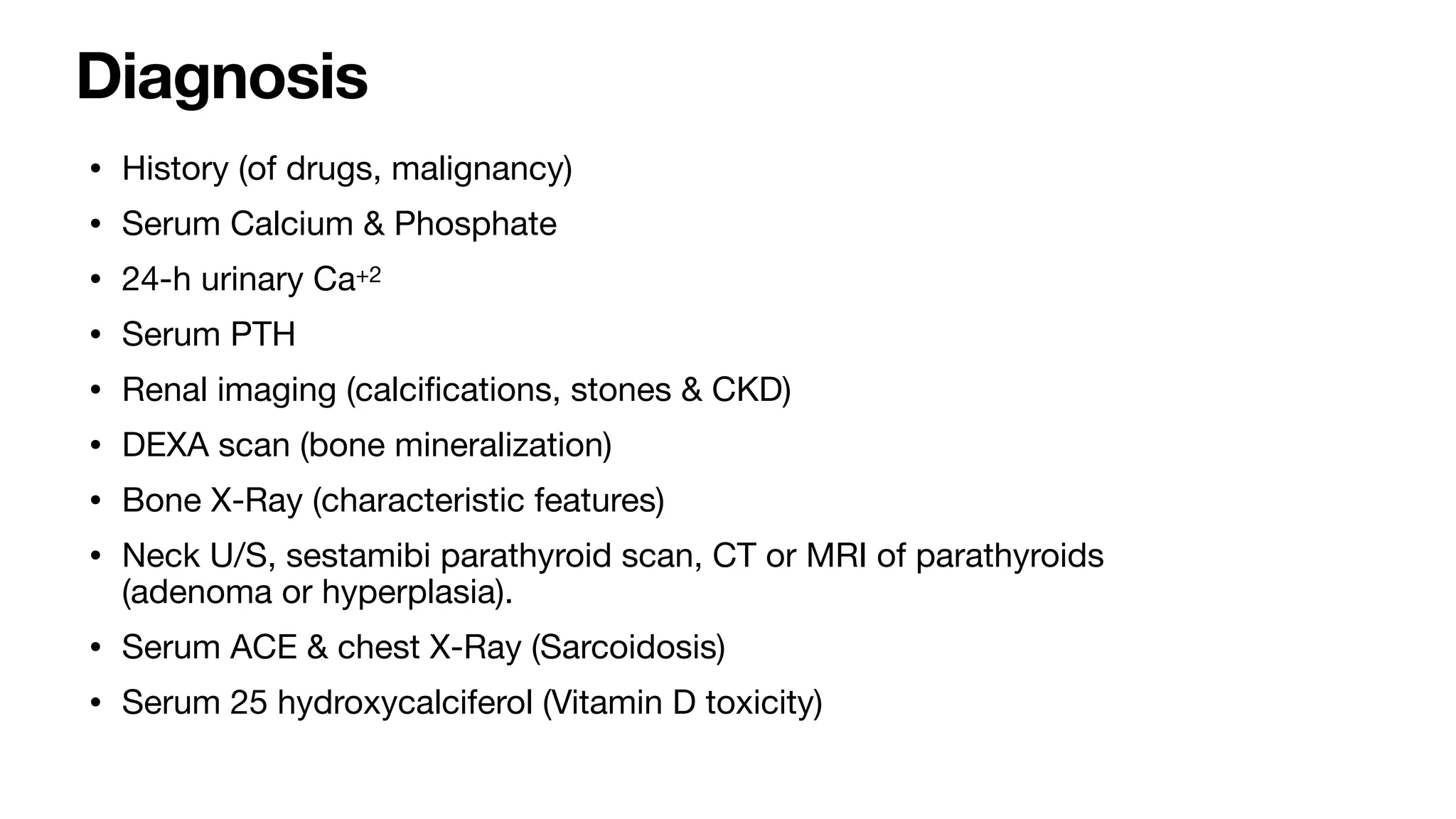
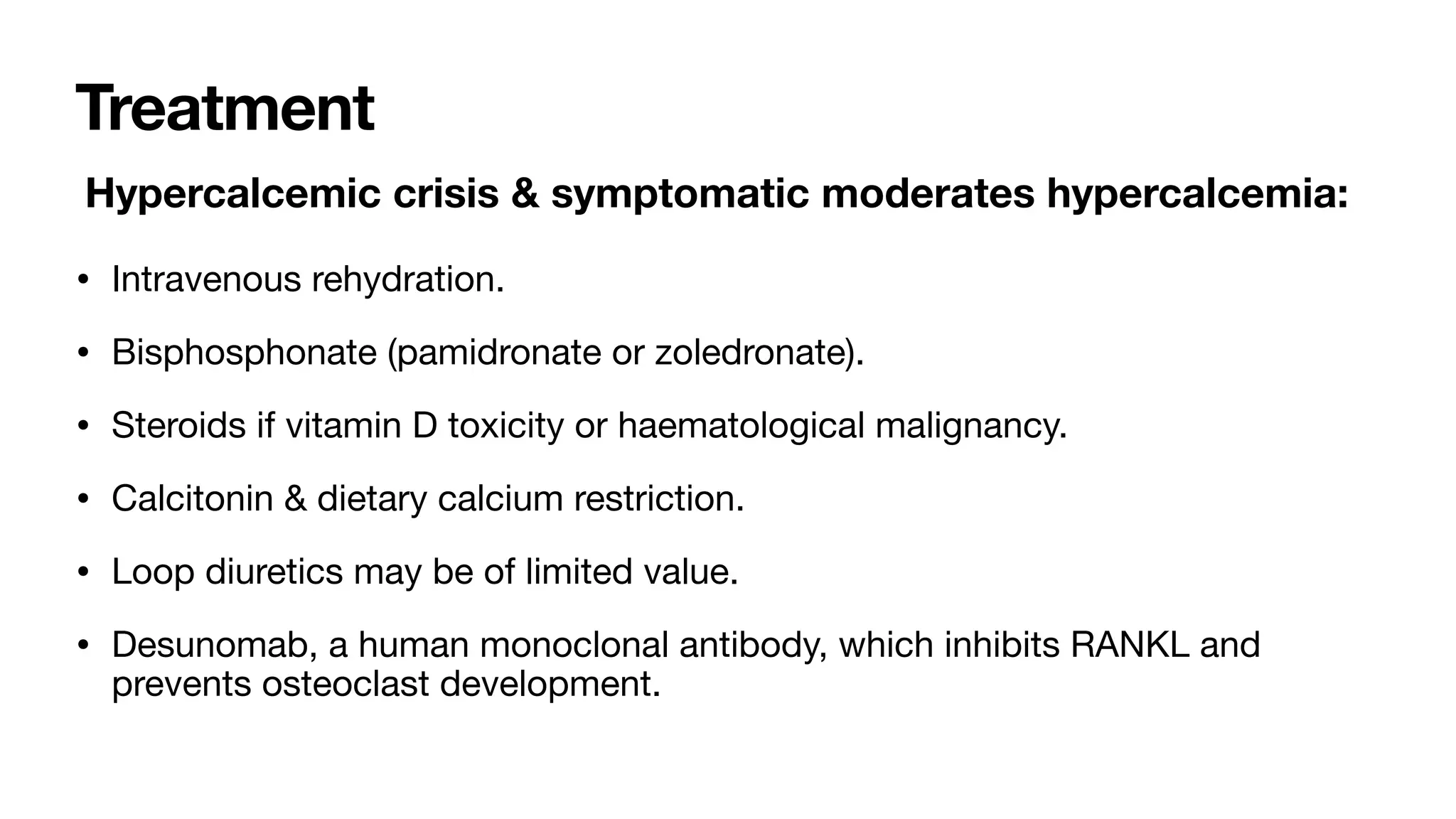
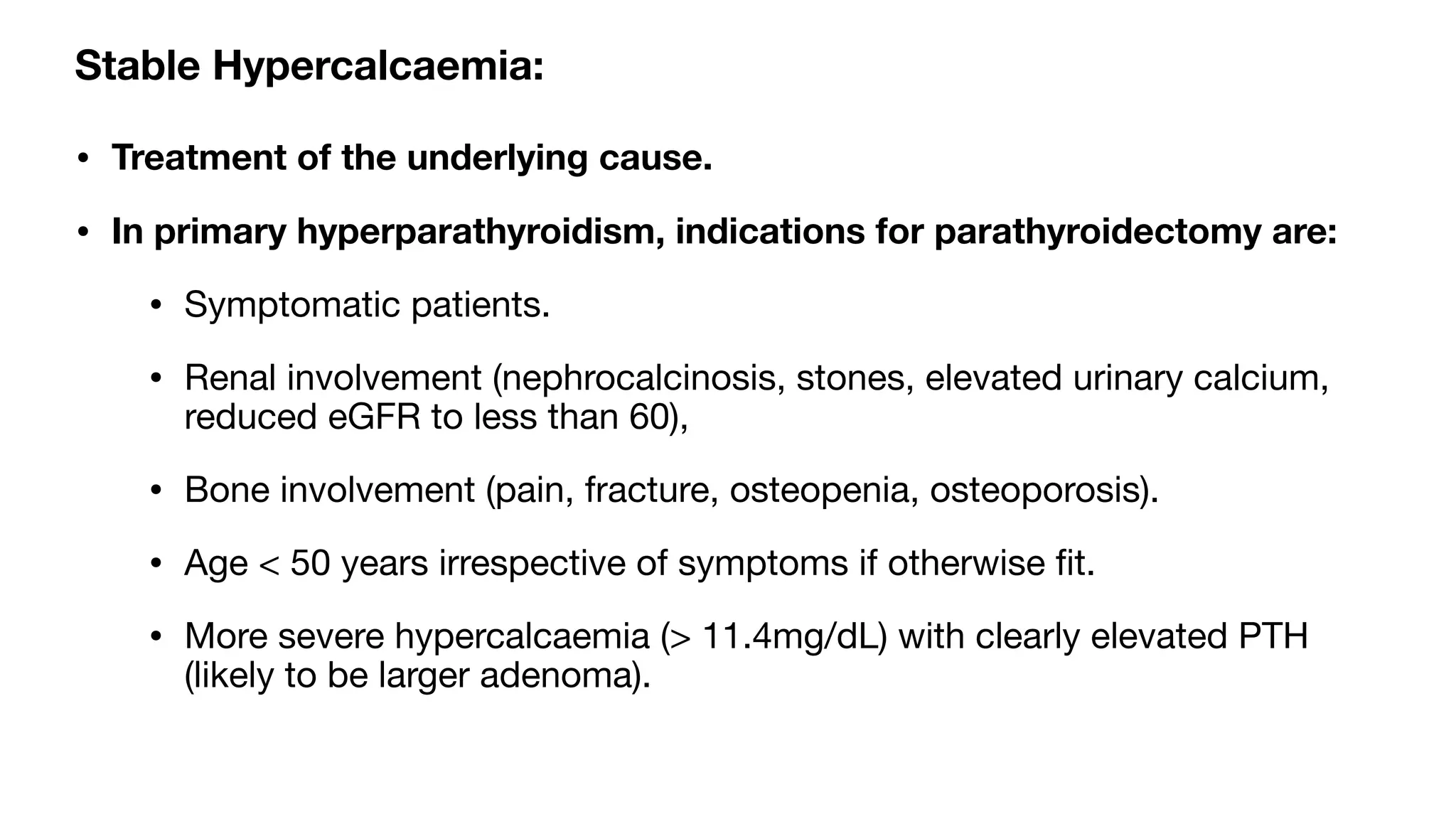
Hypercalcemia is an elevated serum calcium level above the normal range of 8.8-10.4 mg/dL. It can be mild, moderate, or severe/a hypercalcemic crisis if above 14 mg/dL. Common causes include primary hyperparathyroidism, malignancy, and certain drugs. Symptoms range from fatigue and nausea to renal stones, cardiac arrhythmias, and confusion. Diagnosis involves blood and urine tests to determine the calcium and PTH levels and identify the underlying cause. Treatment depends on the severity but may include intravenous fluids, bisphosphonates, surgery for hyperparathyroidism, and treating the underlying condition.