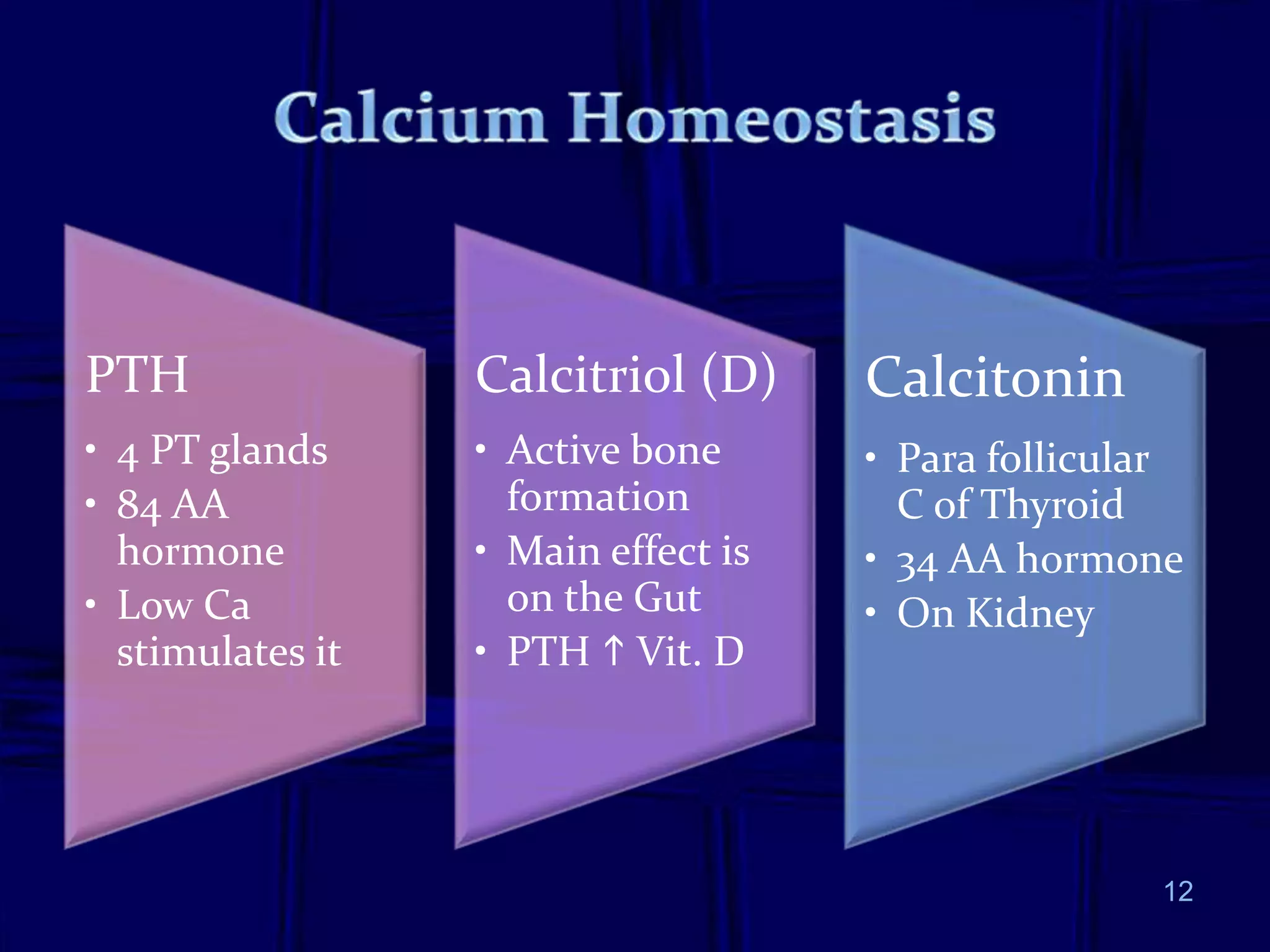
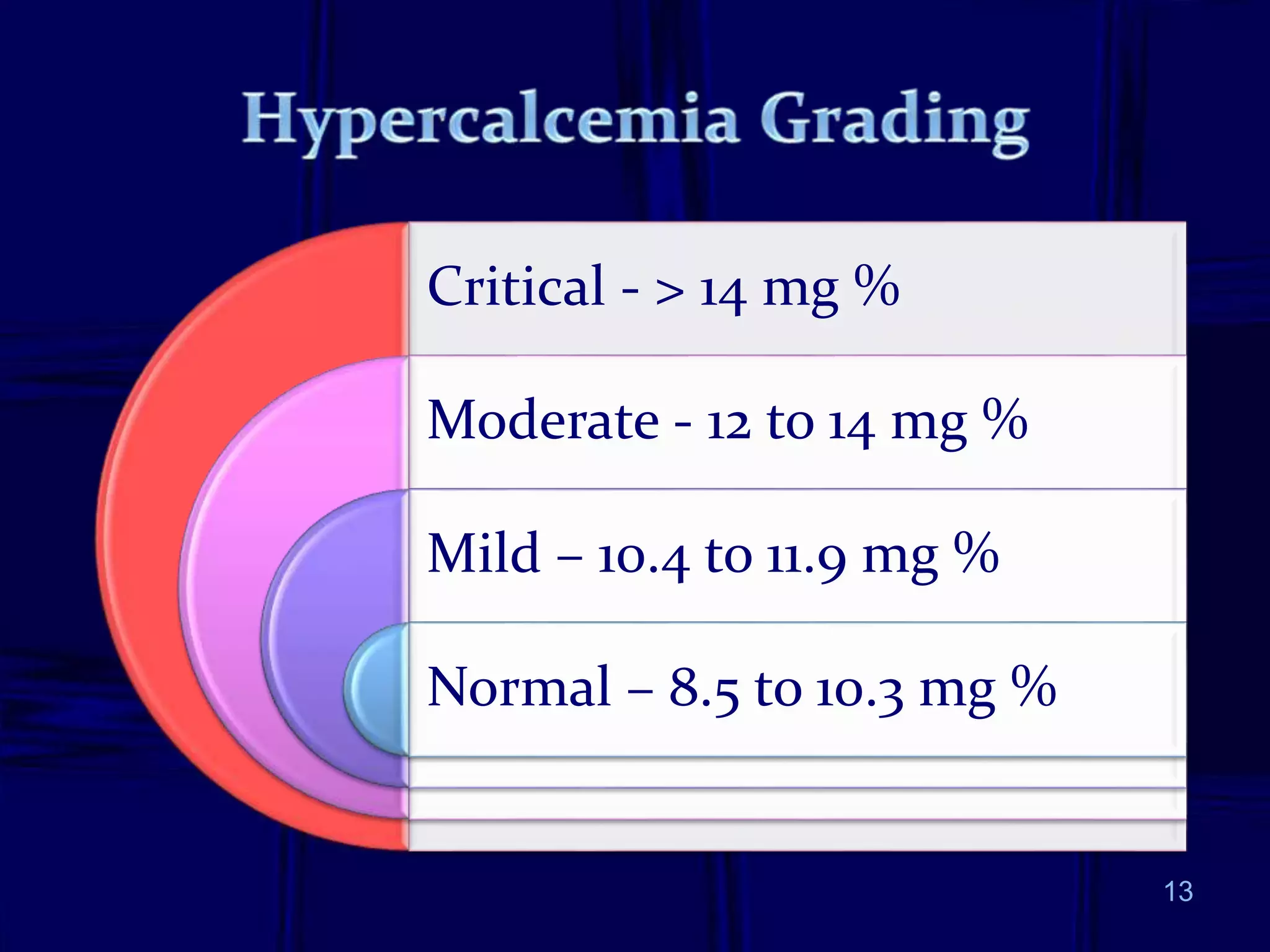
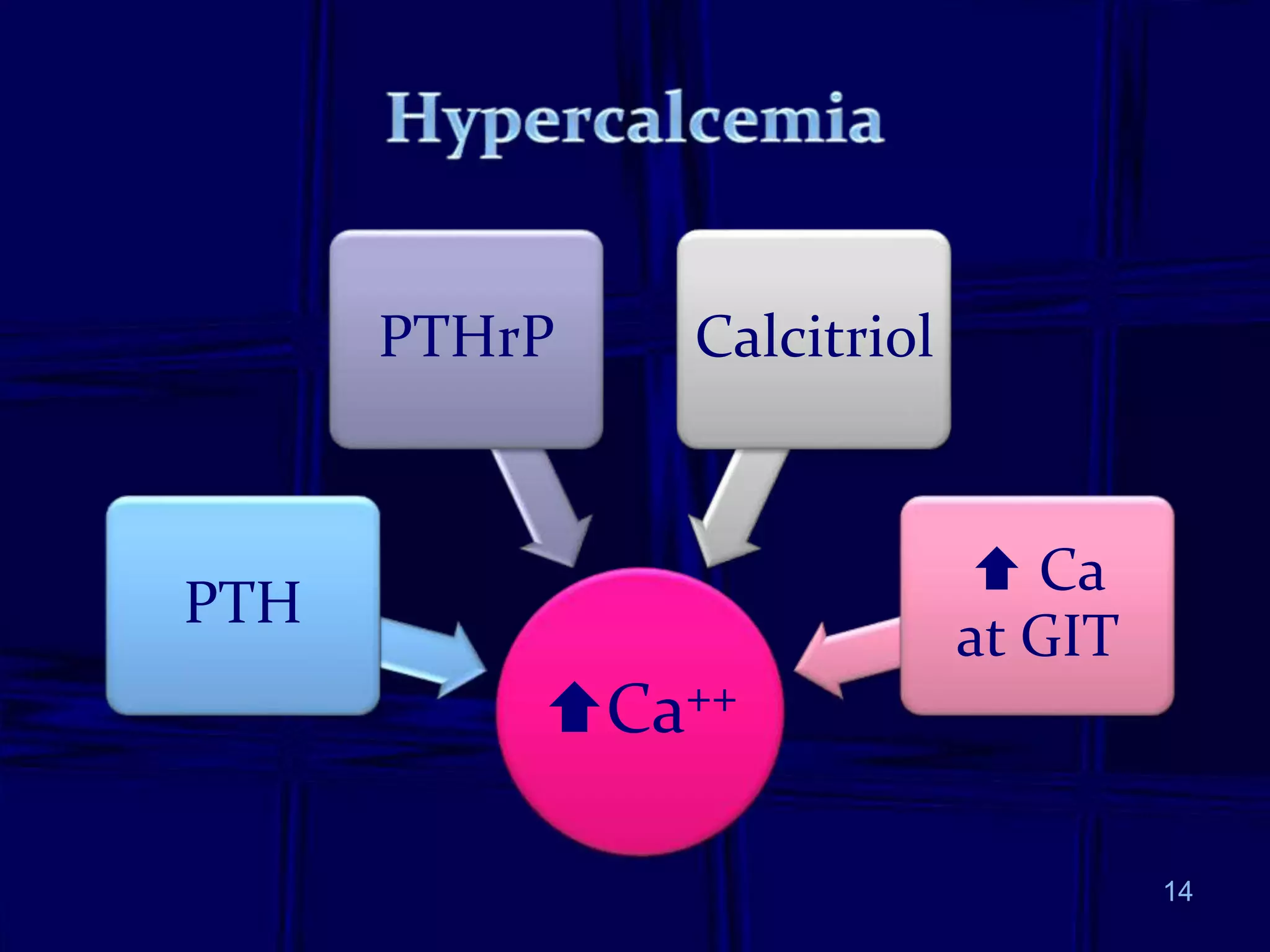
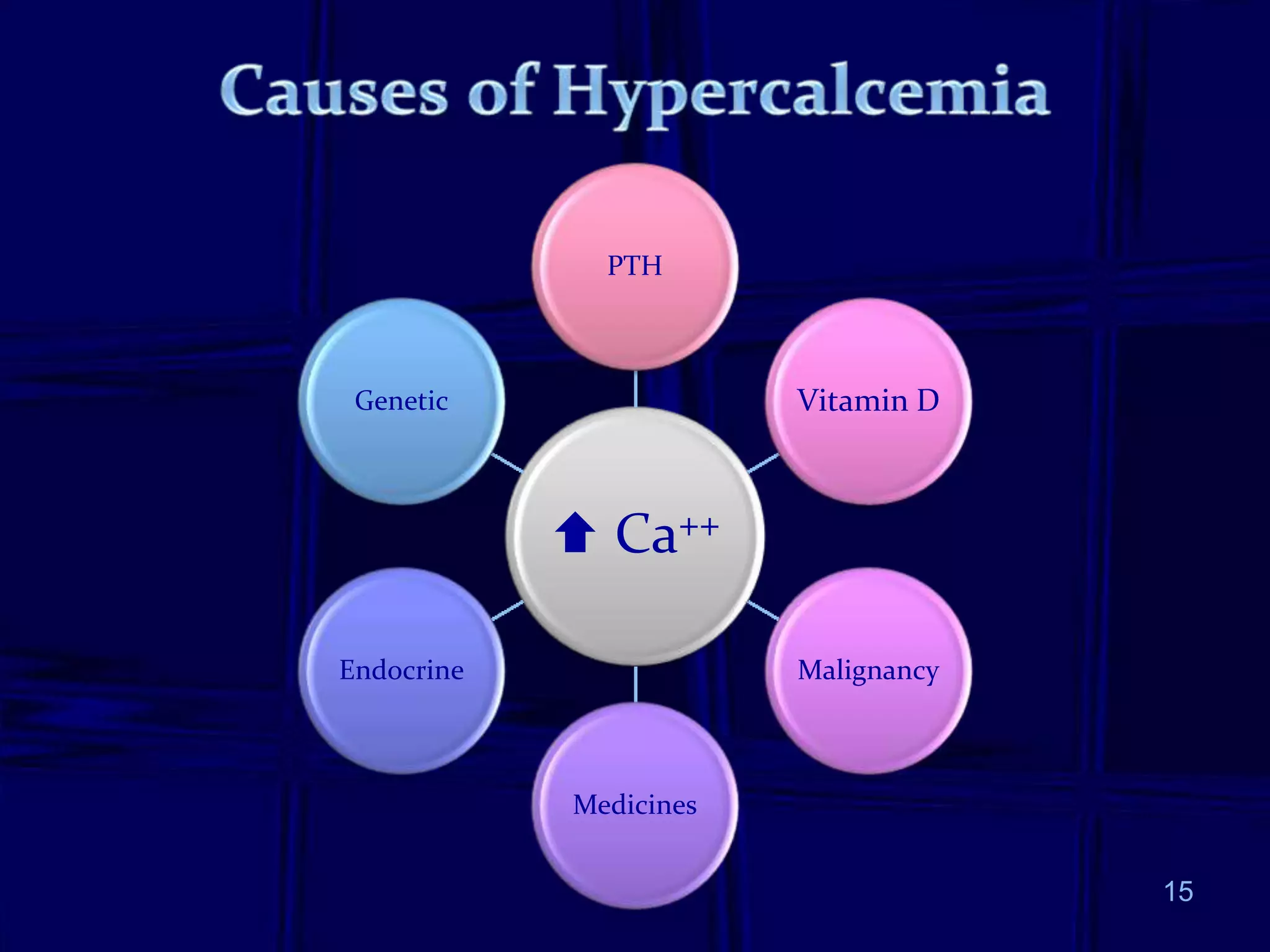
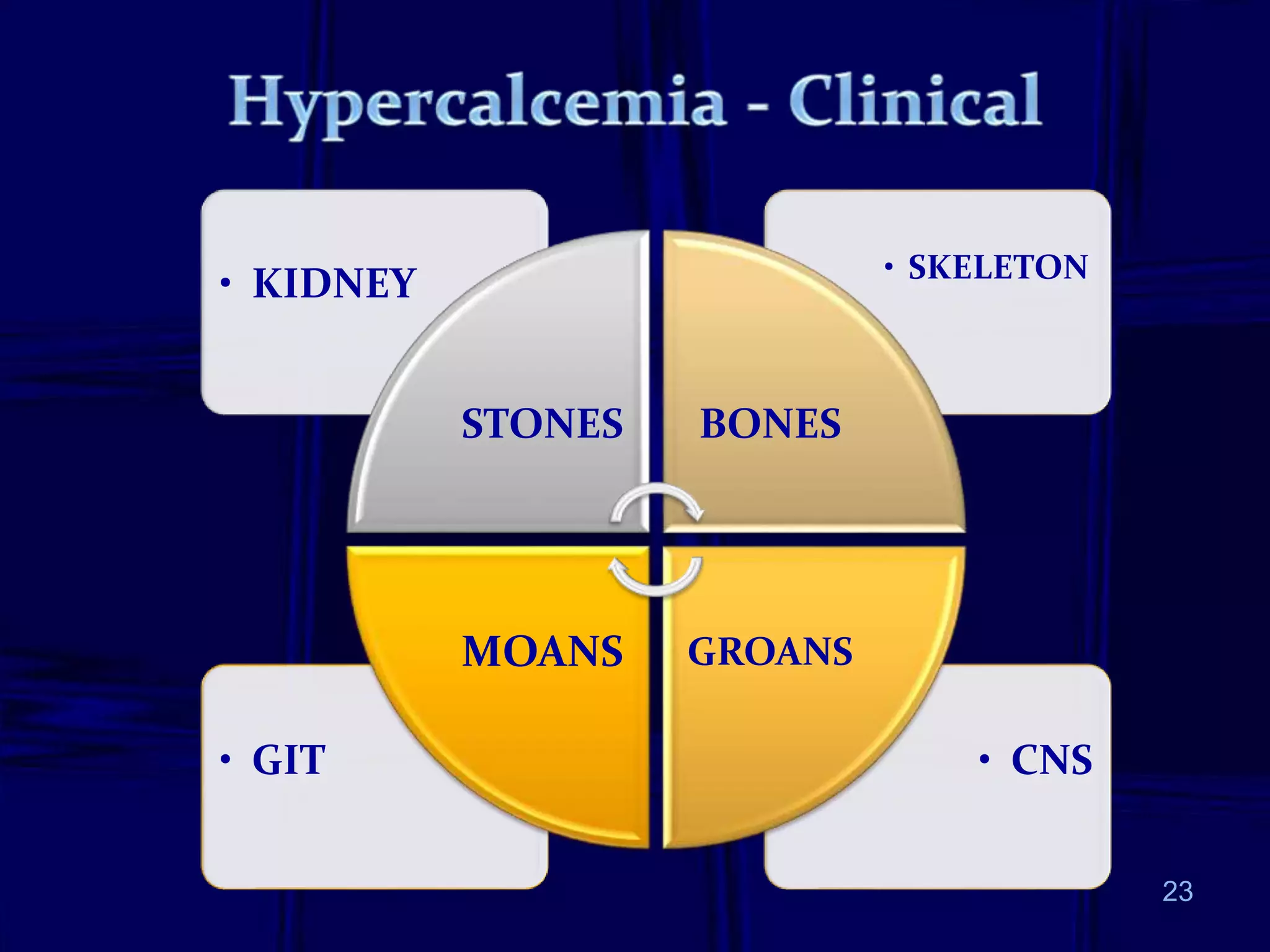
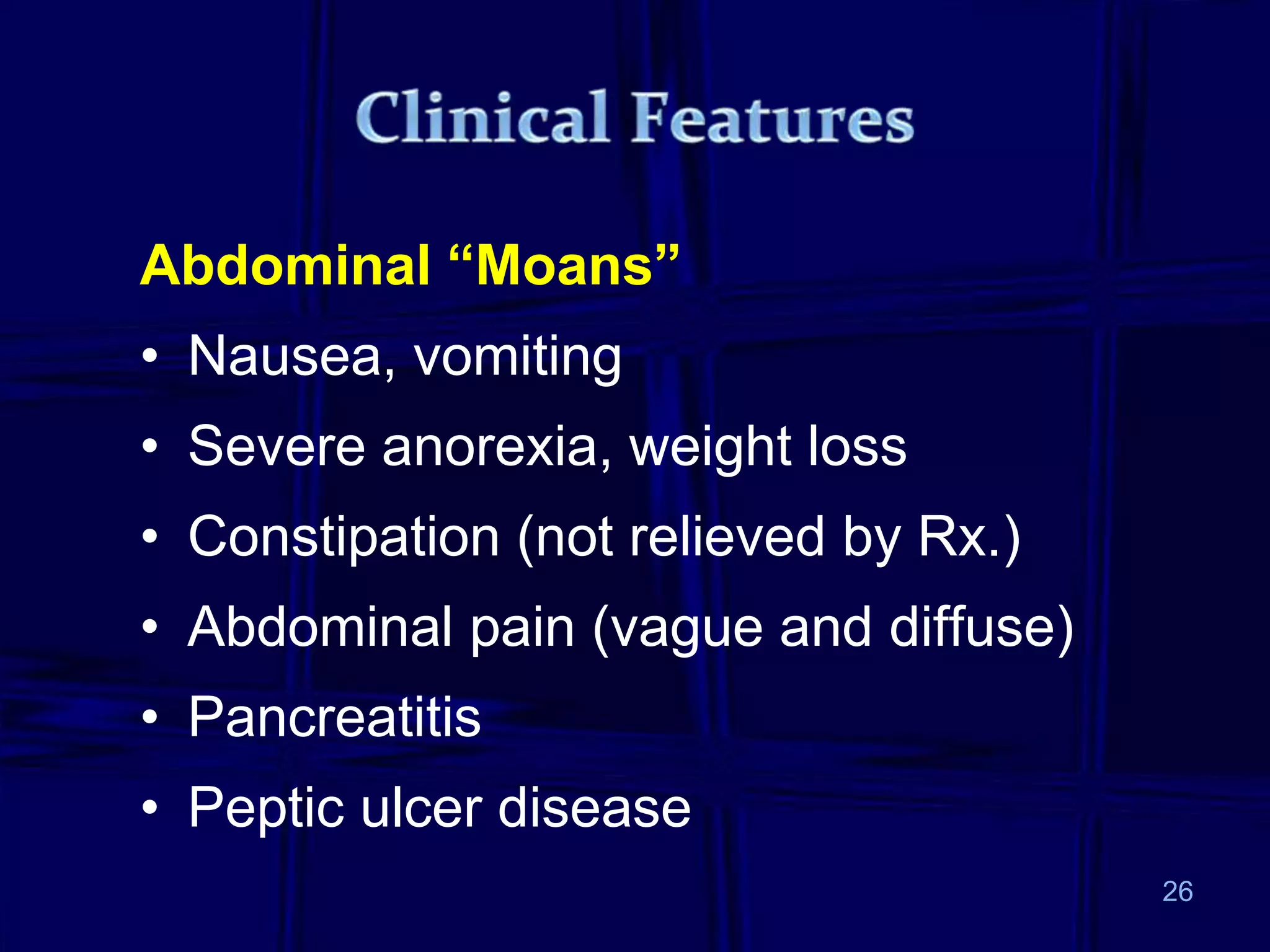
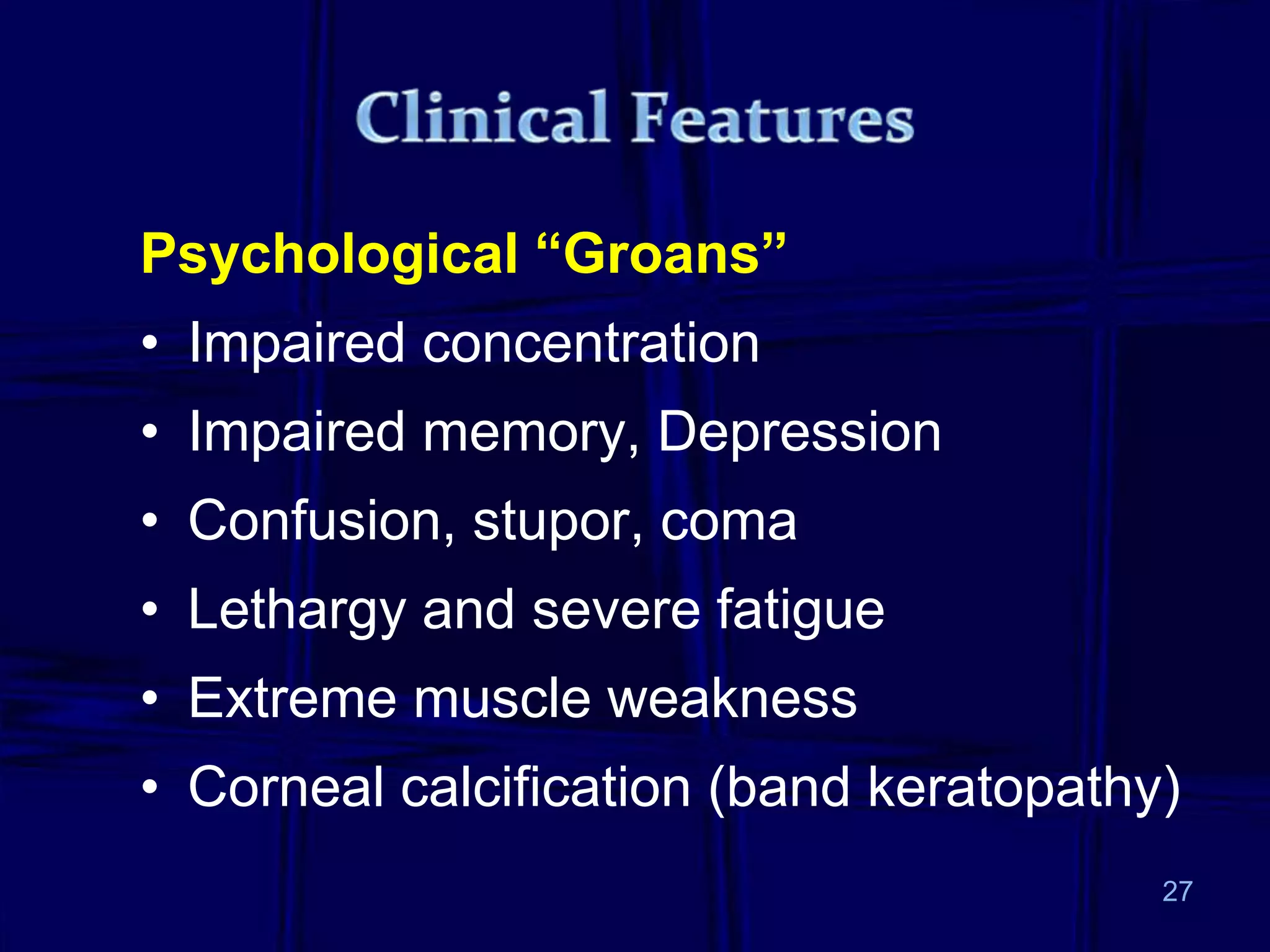
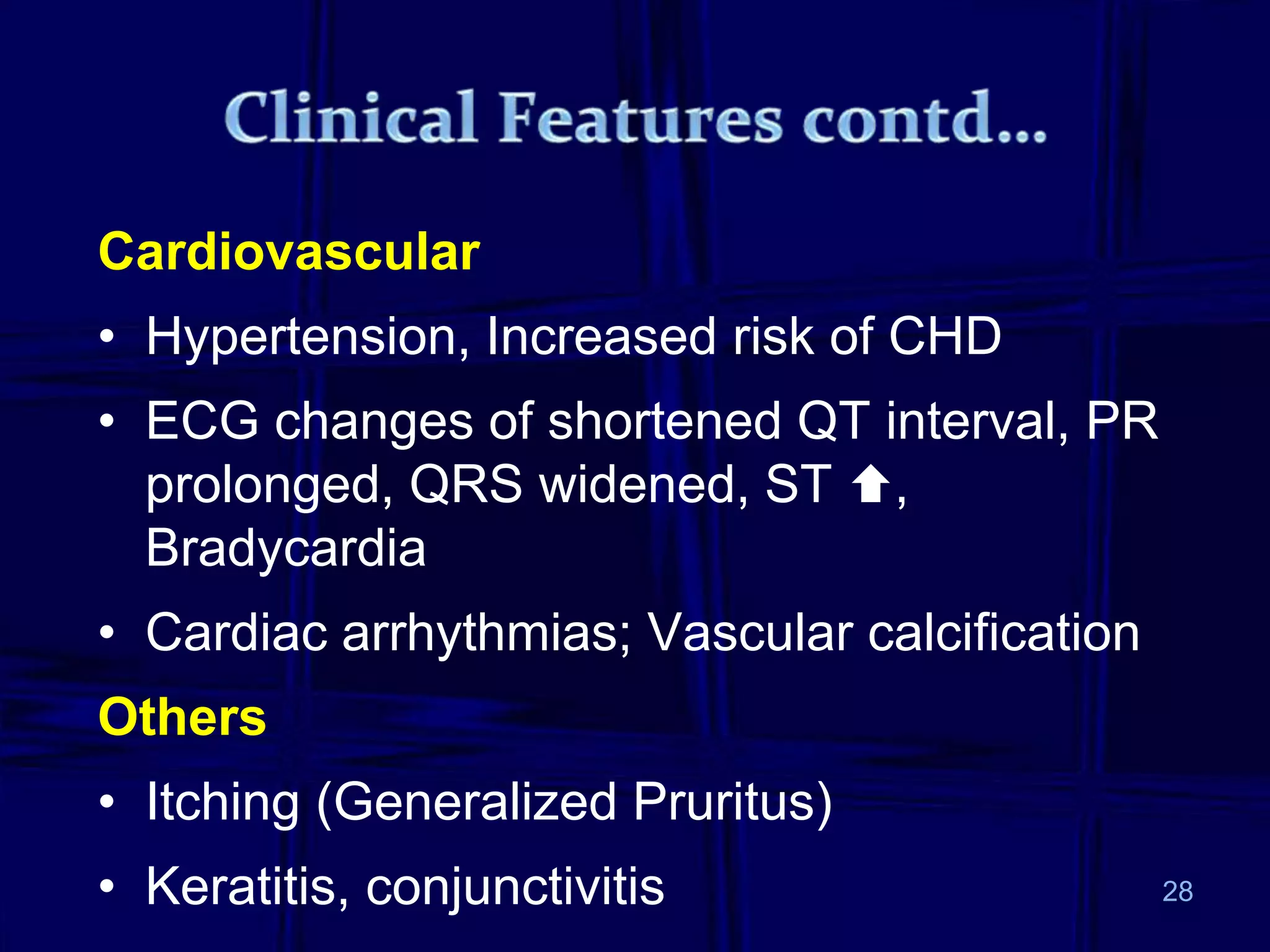
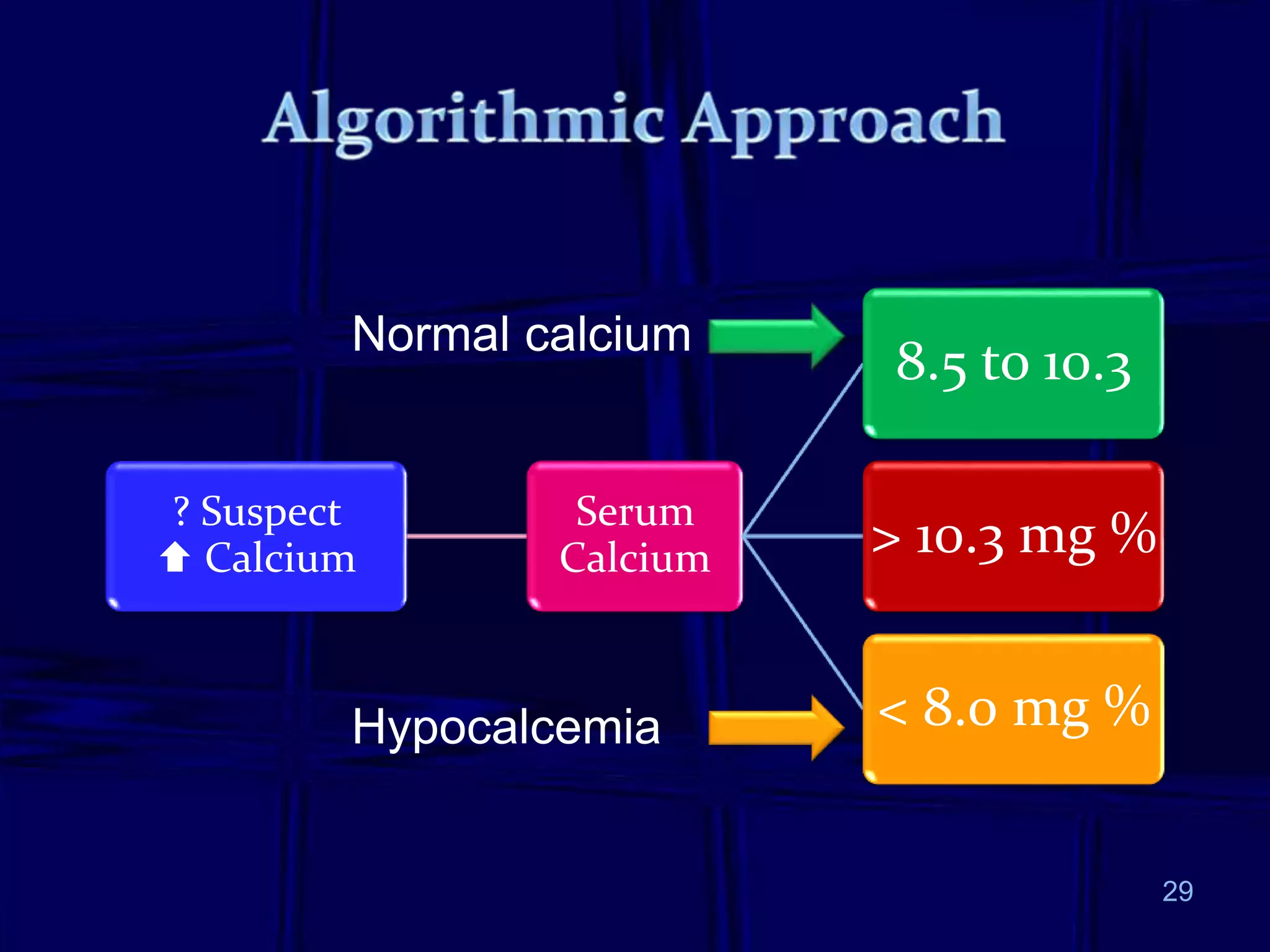
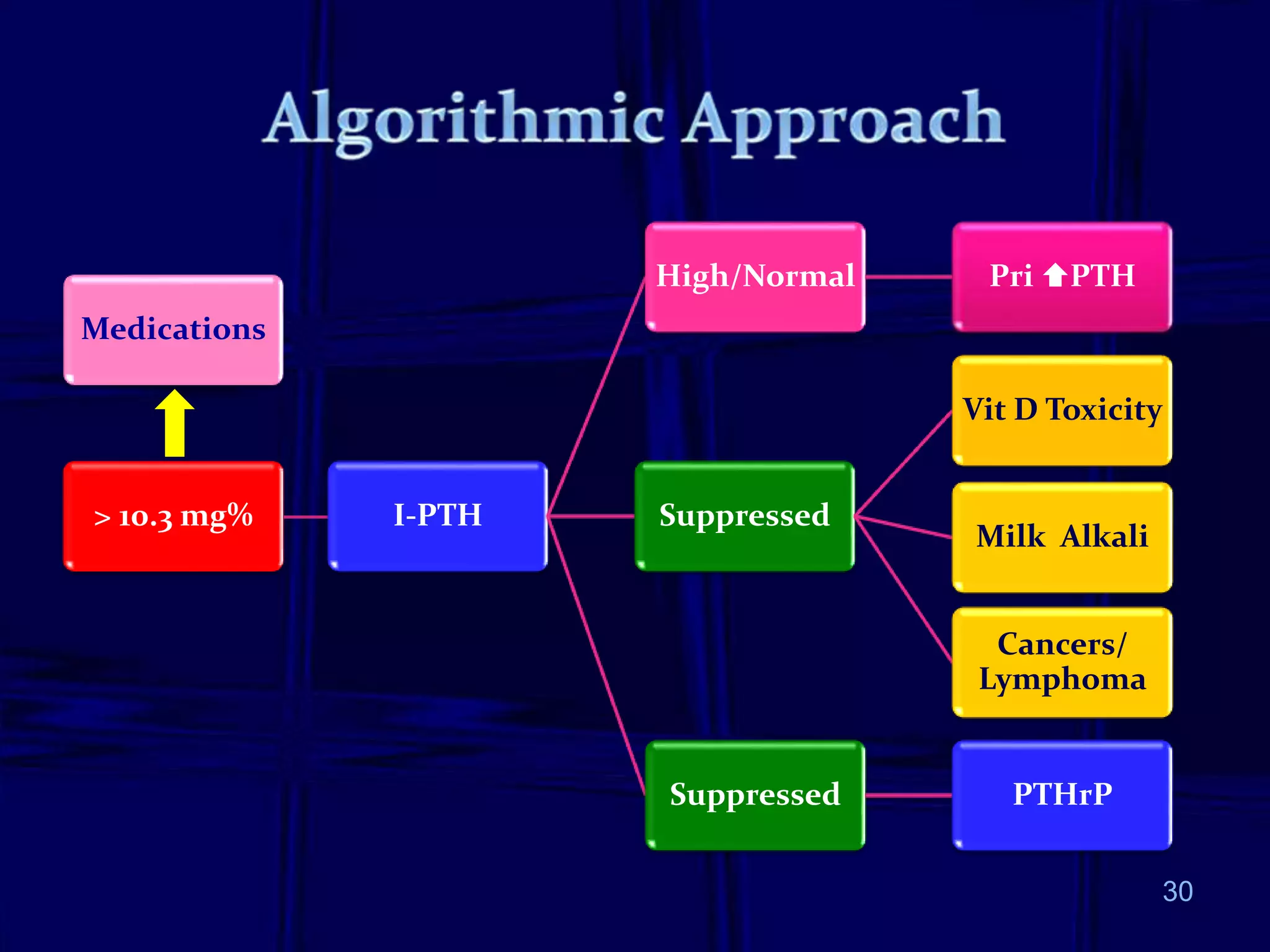
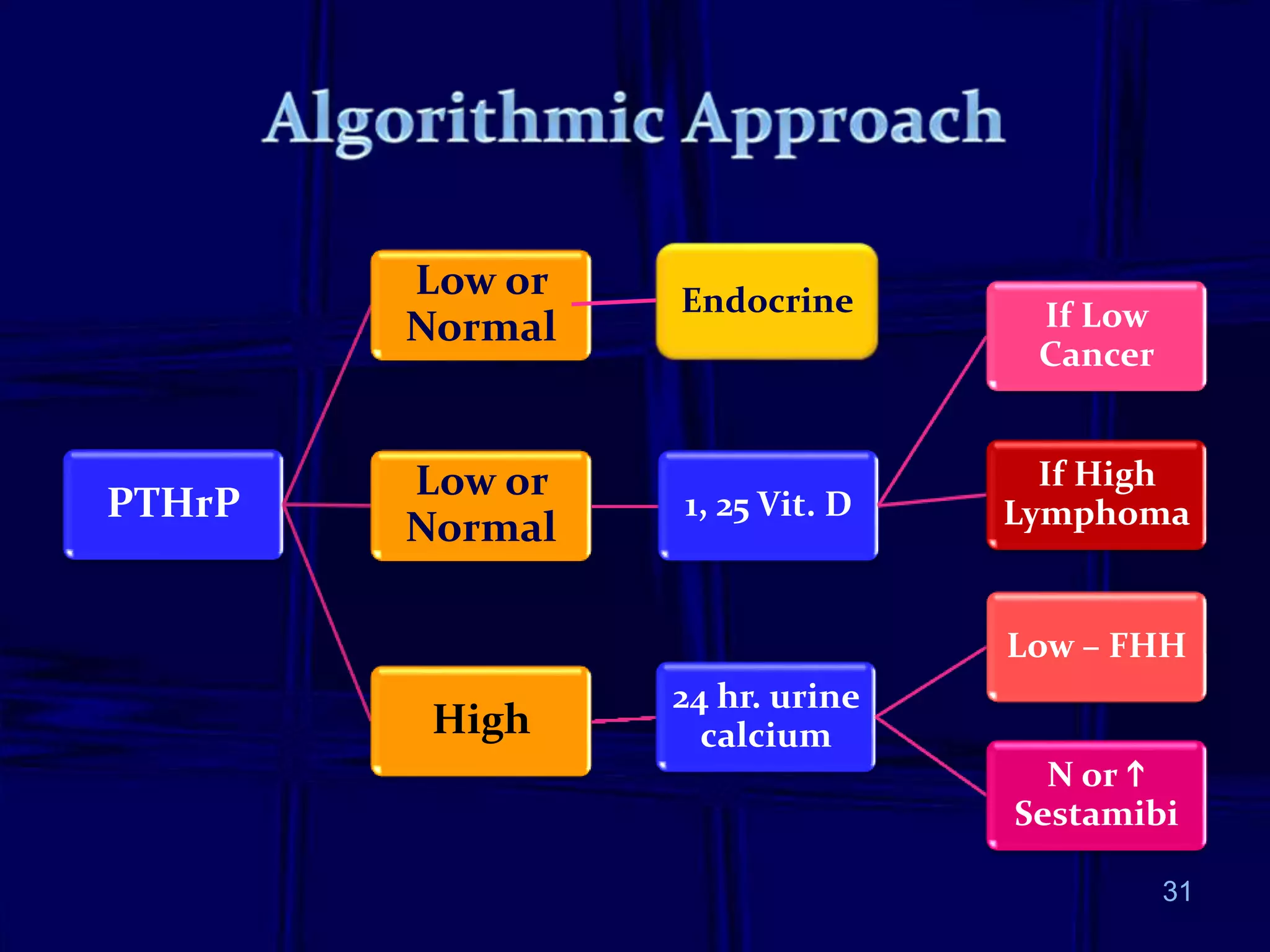
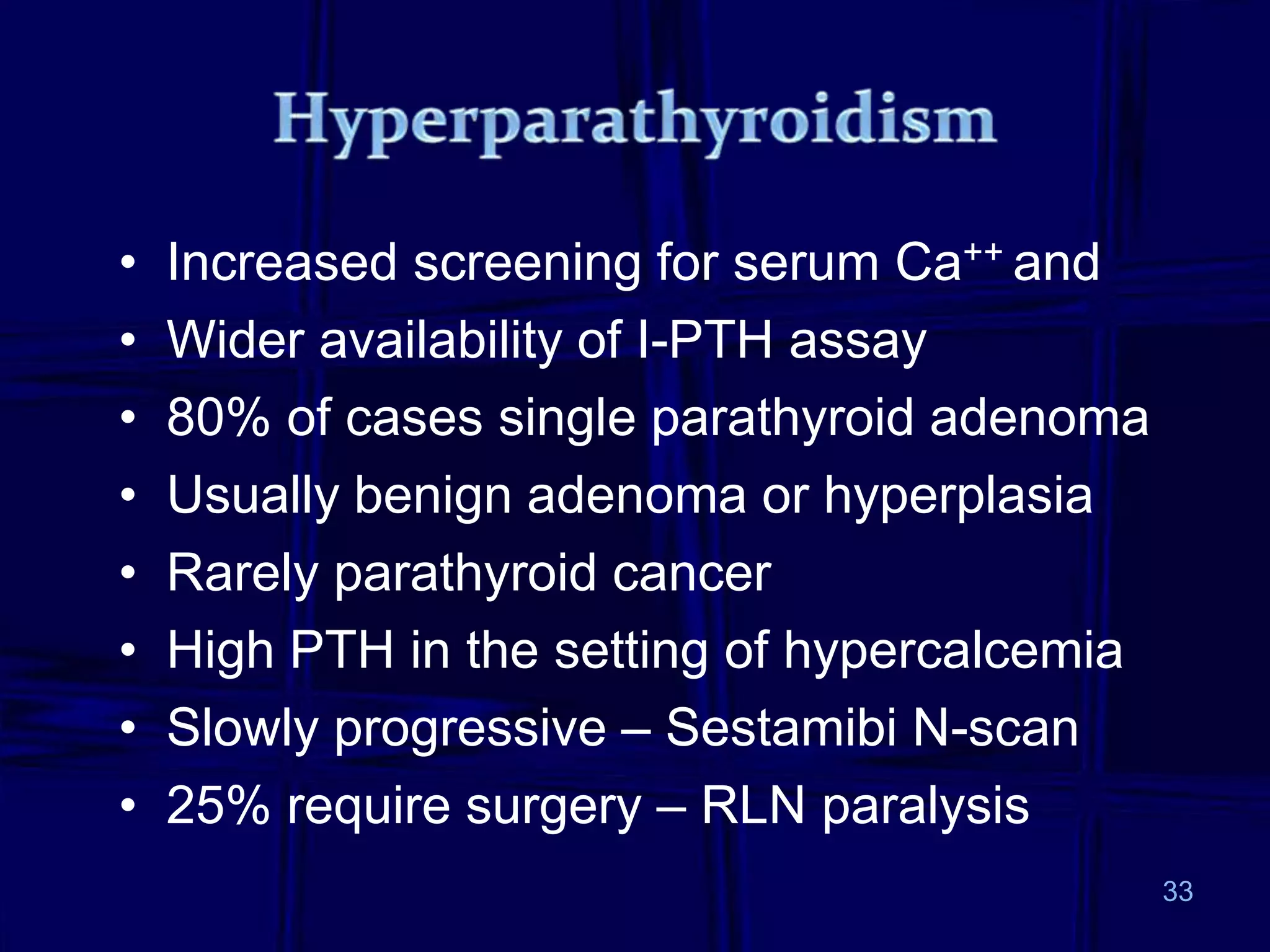
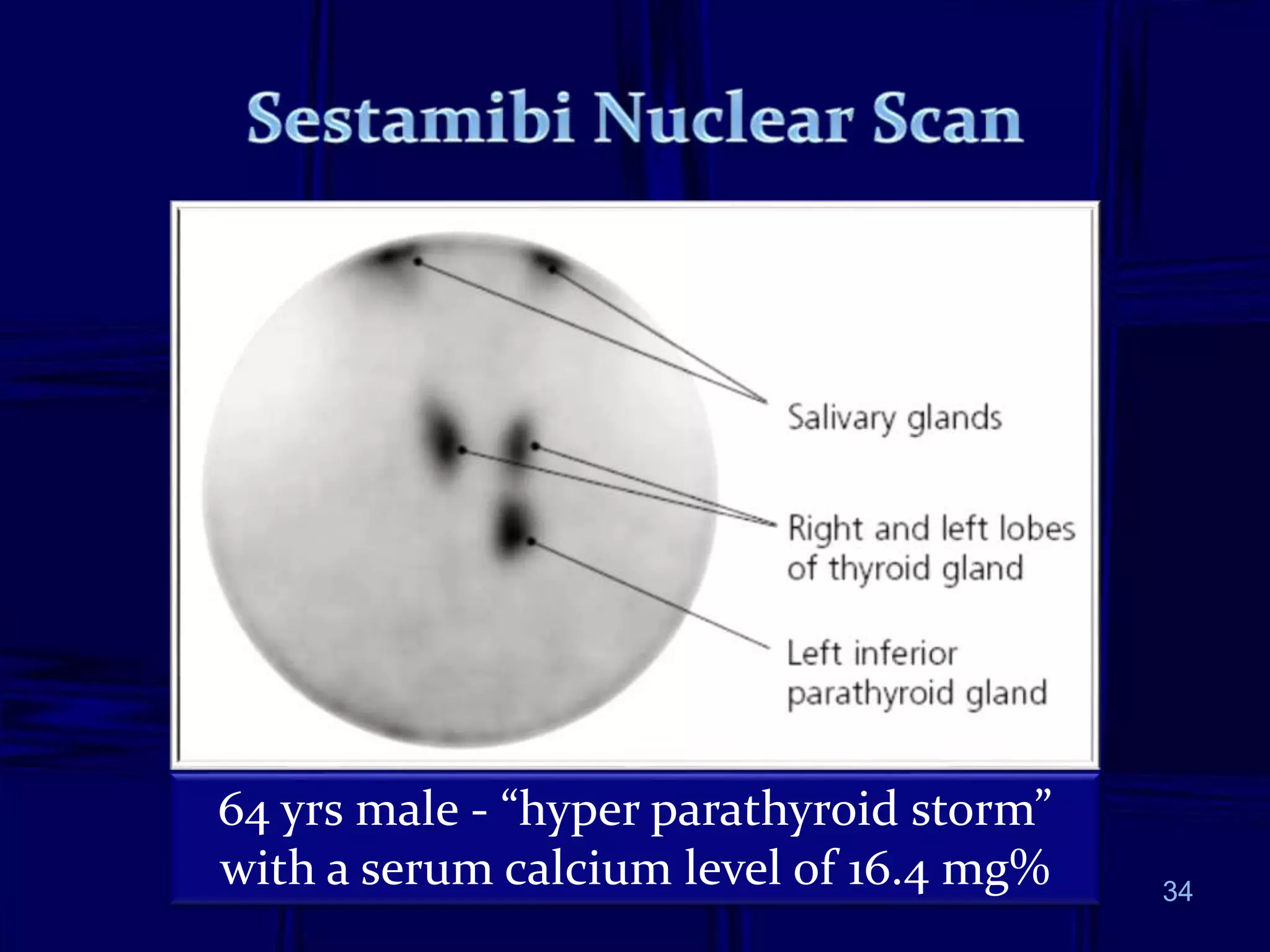
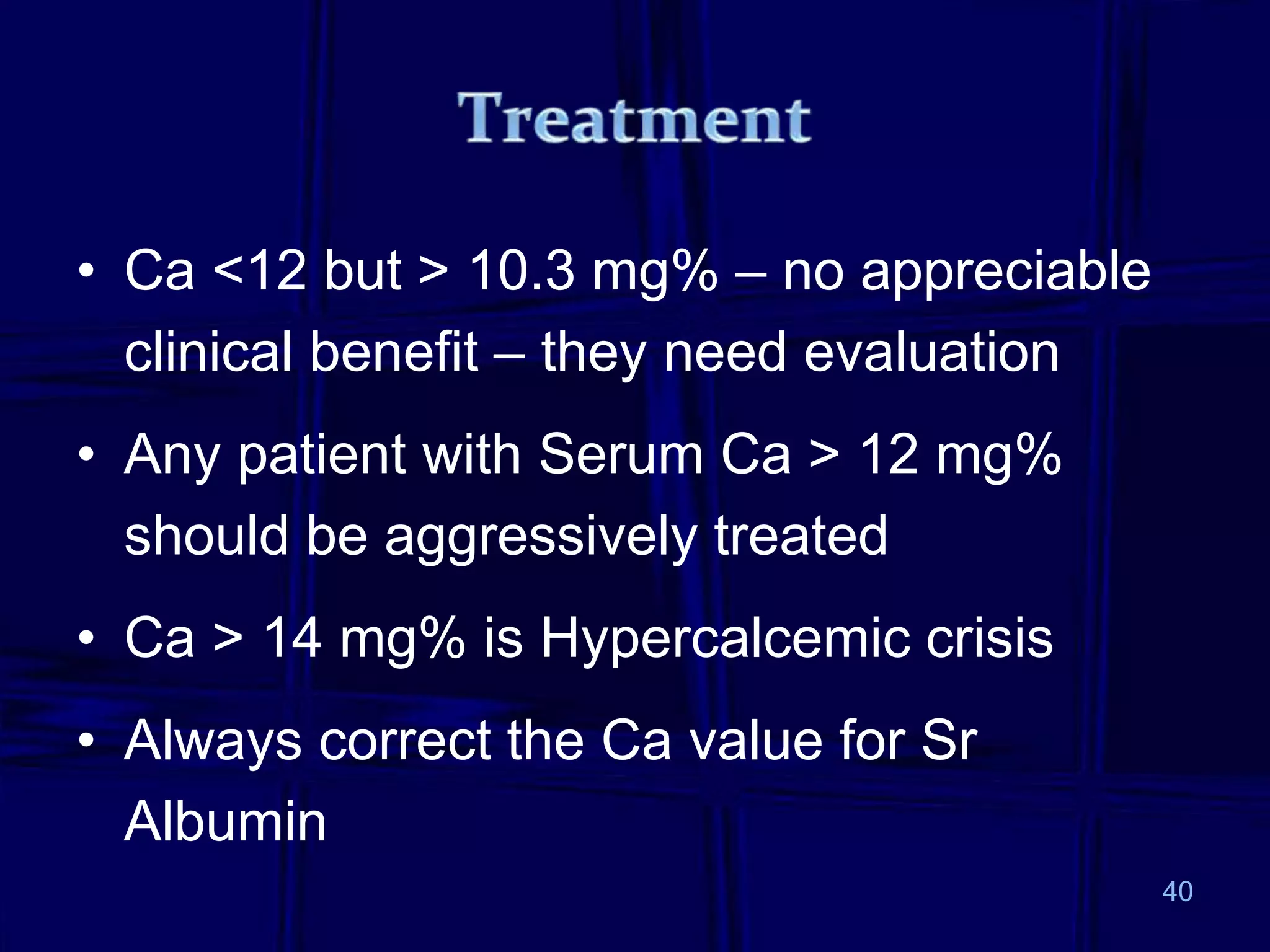
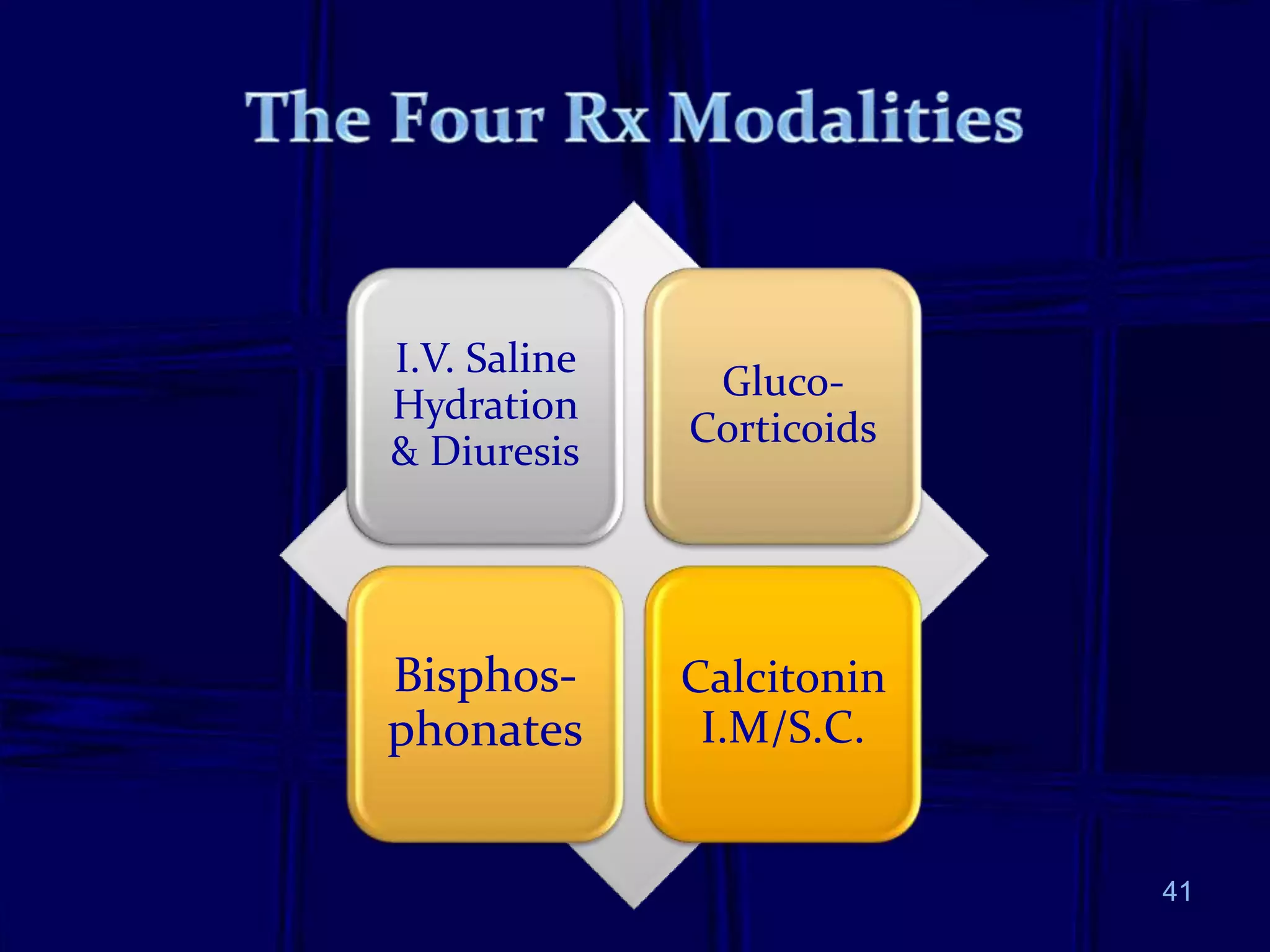
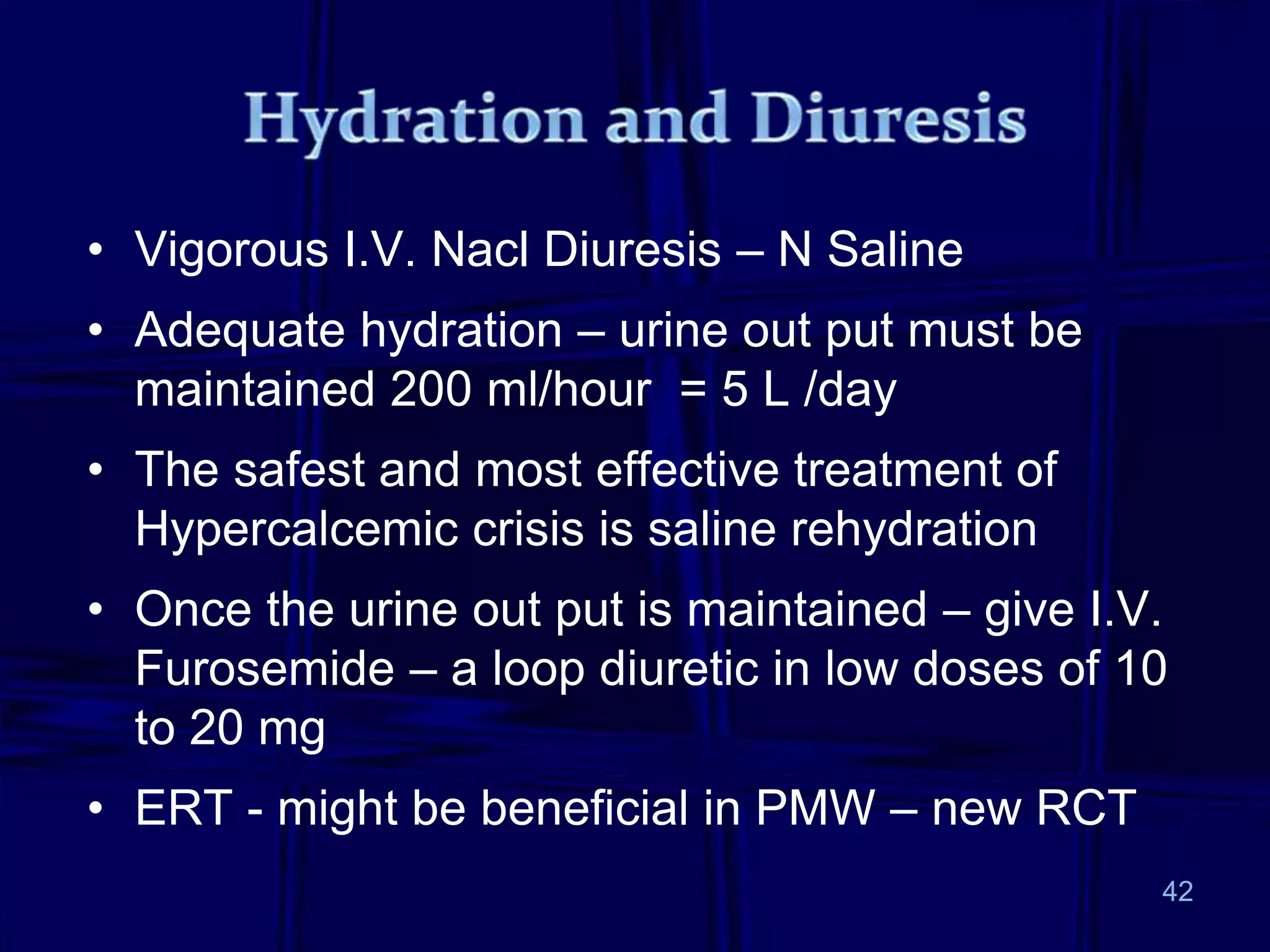
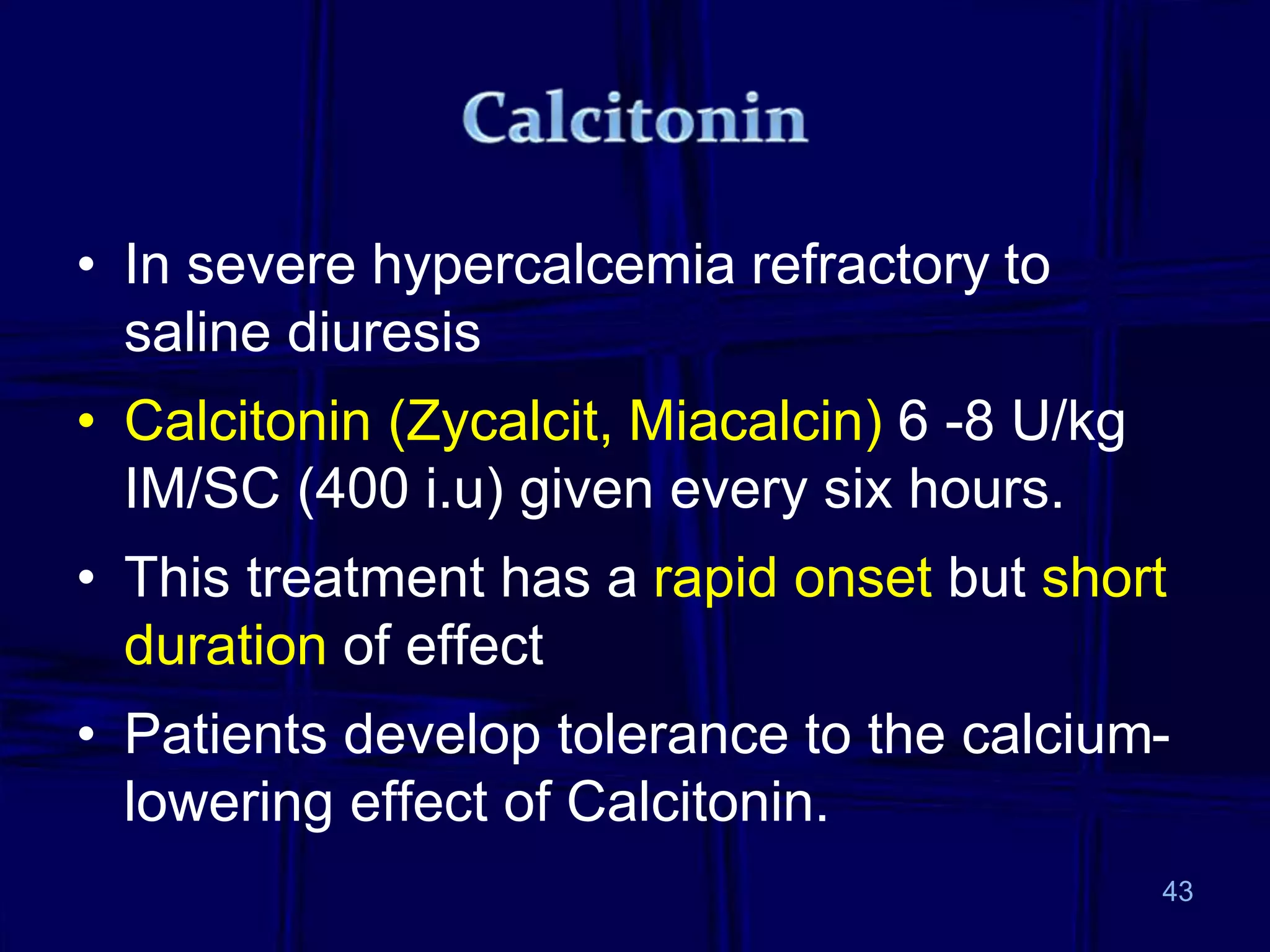
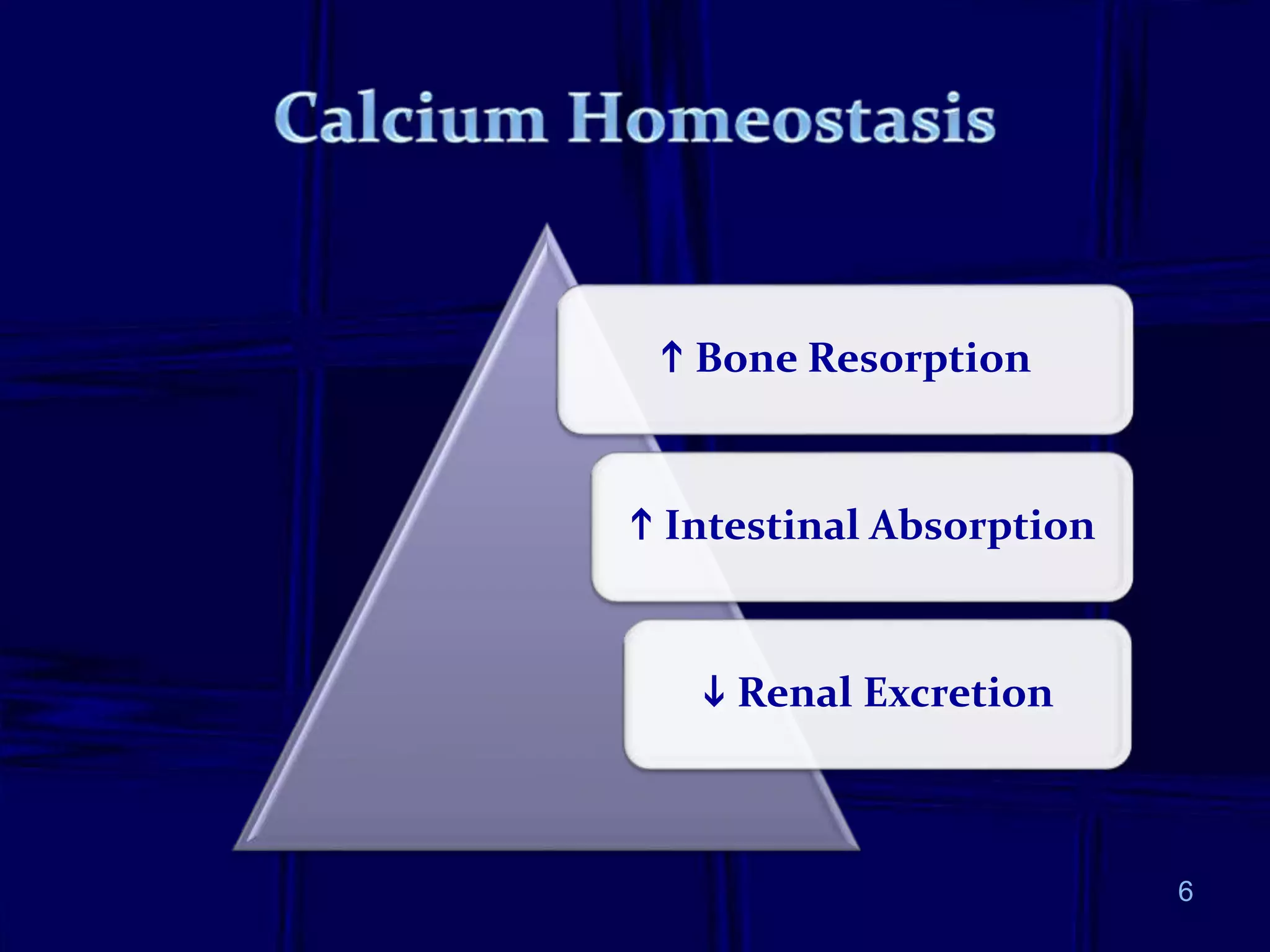
- The document discusses evaluation and management of hypercalcemia. The most common causes are primary hyperparathyroidism and malignancy. Diagnostic workup includes serum calcium, PTH, and history of medications. Hypercalcemic crisis is a medical emergency requiring aggressive intravenous hydration and diuretics, calcitonin, bisphosphonates, or dialysis. Optimal treatment involves identifying and addressing the underlying cause of hypercalcemia.

![Corrected total calcium (mg%) =
[(Measured total calcium mg%) +
{(4.4 - measured albumin g%) x 0.8}]
Example:
[12.0 + {(4.4 – 2.4) x 0.8}] =
[ 12.0 + (2 x 0.8)] = 12.0 + 1.6 = 13.6
mg%
9](https://image.slidesharecdn.com/hypercalcemia-230329060818-c8b1a8f8/75/Hypercalcemia-ppt-9-2048.jpg)