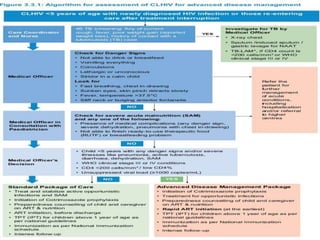
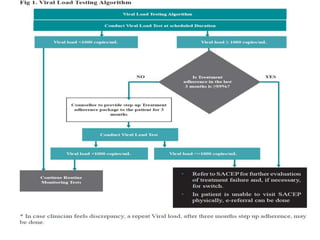
This document discusses HIV in pediatrics. It describes the two types of HIV, HIV-1 being most common worldwide. It outlines the WHO clinical staging of HIV in adolescents and children from Stage 1 (asymptomatic) to Stage 4 (severe manifestations). It discusses diagnosis of HIV infection in infants and children, including early infant diagnosis using viral RNA or antigen detection. It covers ART goals, considerations before initiation, groups and classes of drugs used, monitoring after initiation and management of treatment failure in children living with HIV. Key counseling issues for child clients and their parents/caregivers are also summarized.