This document provides an overview of headaches, including their prevalence, causes, classification, diagnosis, and management. Some key points:
- Headaches are one of the most common health complaints worldwide, affecting up to 90% of people in a given year.
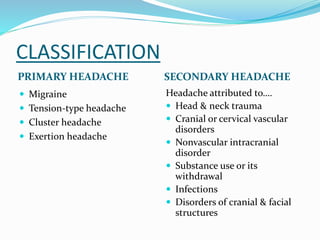
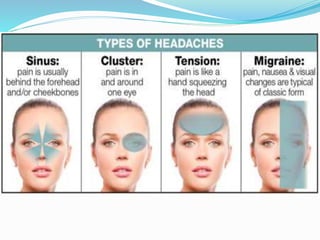
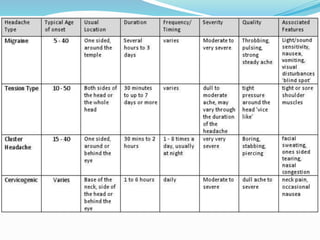
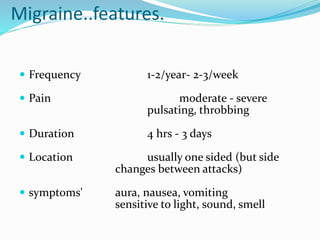
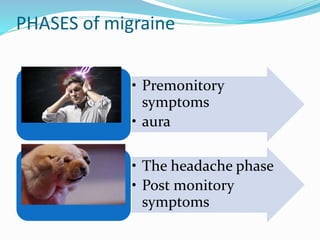
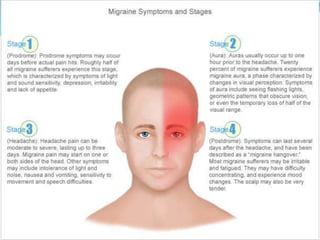
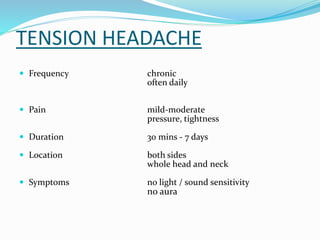
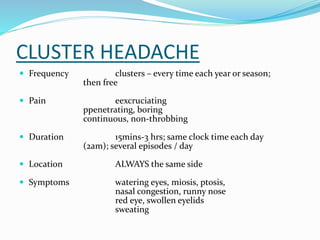
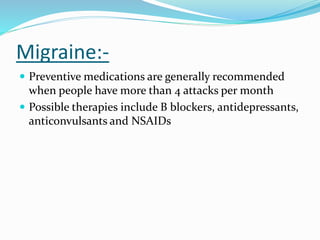
- Headaches can be primary (e.g. migraines, tension-type) or secondary due to other causes like head trauma.
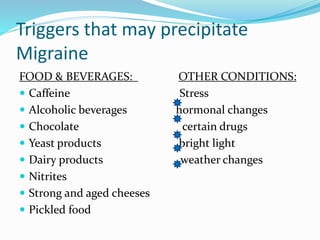
- Diagnosis is based on patient history. Management involves analgesics, preventative medications, and lifestyle changes like stress management.
- New treatments include biofeedback, Botox injections, and neuromodulation techniques like transcranial magnetic stimulation.