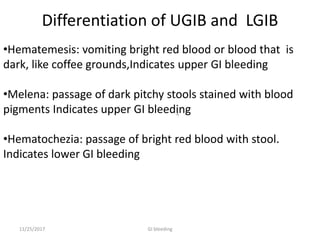
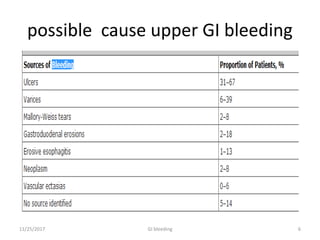
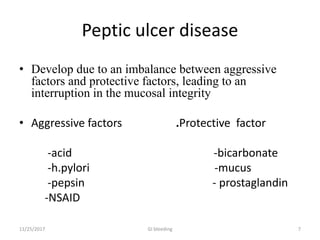
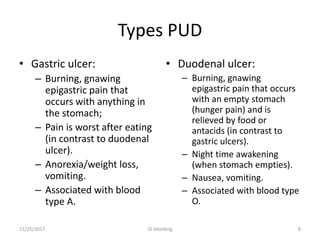
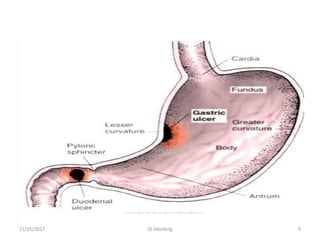
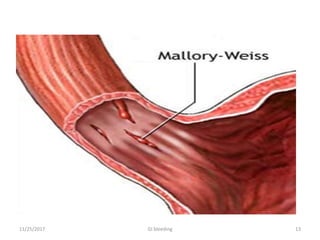
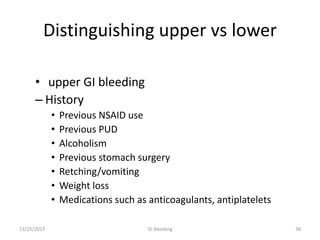
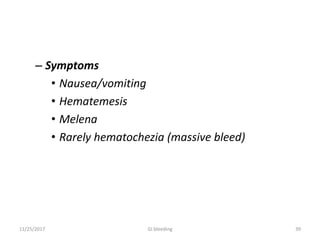
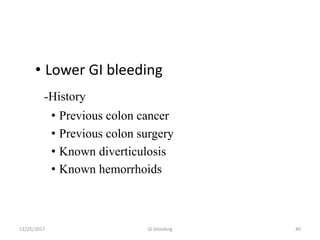
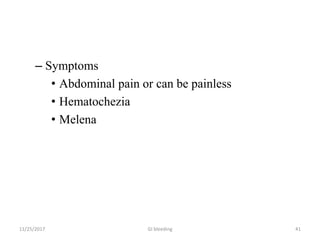
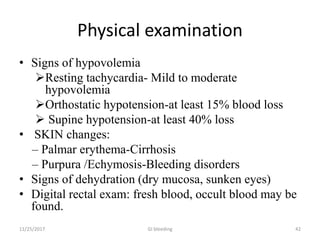
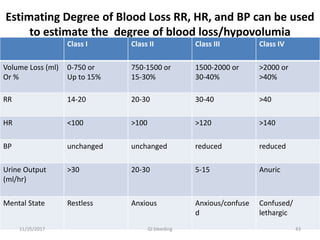
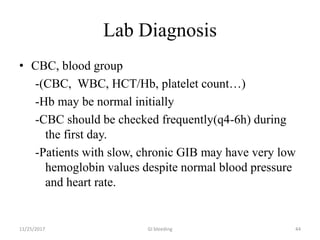
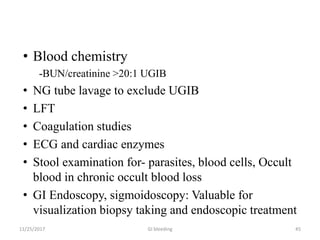
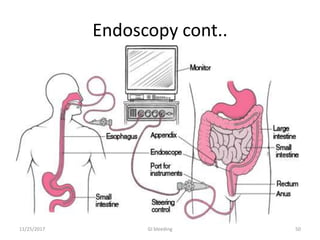
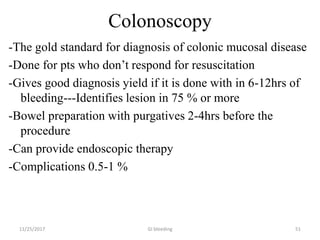
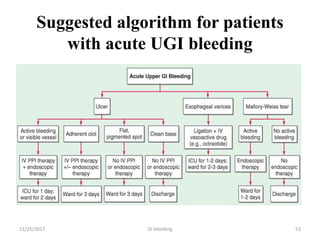
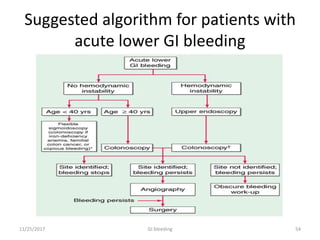
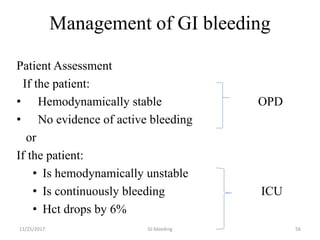
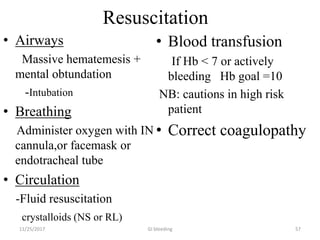
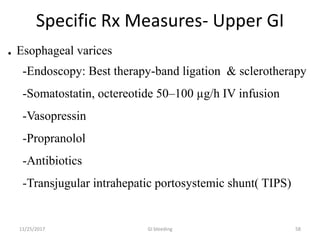
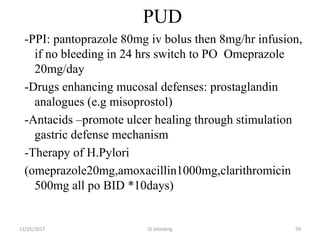
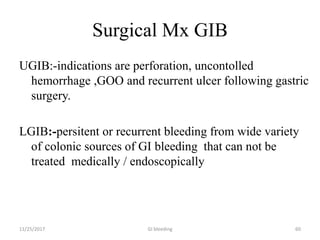
Upper GI bleeding accounts for nearly 80% of significant gastrointestinal bleeding. Common causes of upper GI bleeding include peptic ulcer disease, esophageal varices, Mallory-Weiss syndrome, and erosive gastropathy. Lower GI bleeding accounts for about 20% and possible causes include diverticular disease, vascular abnormalities like angiodysplasia, inflammatory conditions, and neoplasms. Evaluation of a patient with GI bleeding involves assessing severity, identifying potential sources, and looking for conditions that may impact management. Initial evaluation includes history, physical exam, and lab tests. Endoscopy allows for diagnosis and potential treatment.