This document is a facilitator's guide for a family planning competency-based training program. It includes an introduction, 12 modules on various topics related to family planning, and appendices. The guide provides information on the objectives and content of the training, the roles of facilitators and participants, evaluation methods, and how to use the training manual. It aims to enable health providers to safely provide and discuss different modern family planning methods with clients.



























































































































































































































![IN MALES
Boys begin the process of puberty at about 10 to 17 years old. The following are the physical
changes during puberty:
1. Testicular size, function, and fertility
This is the first physical manifestation of puberty in males. The testes start producing testosterone
and sperms. Sperm can be detected in the morning urine of most boys after the first year of
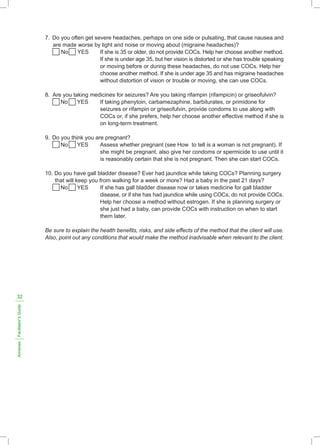
pubertal changes (and occasionally earlier). Potential fertility is reached at about 13 years old
in boys, but full fertility will not be gained until 14 to 16 years of age, although some go through
the process faster, reaching it only a year later.
2. Pubic hair
Pubic hair often appears on a boy shortly after the genitalia begin to grow. The pubic hairs are
usually first visible at the dorsal (abdominal) base of the penis. After another six to 12 months,
the hairs are too many to count and which become more dense to fill the "pubic triangle". These
also spread to the thighs and upward towards the navel, as part of the developing abdominal
hair.
3. Body and facial hair
In the months and years following the appearance of pubic hair, other areas of skin which
respond to androgens (testosterone) develop heavier hair in roughly the following sequence:
underarm (axillary) hair, perianal hair, upper lip hair, sideburn (preauricular) hair, periareolar
hair, and the rest of the beard area. Arm, leg, chest, abdominal, and back hair become heavier
more gradually.
There is a large range in amount of body hair among adult men, and significant differences in
timing and quantity of hair growth among different ethnic groups.[13]
Chest hair may appear during puberty or years after. Not all men have chest hair.
4. Voice change
Under the influence of androgen, the voice box, or larynx, grows in both sexes. This growth
is far more prominent in boys, causing the male voice to drop and deepen. This sometimes
occurs abruptly but rarely "overnight," by about one octave. Full adult pitch is attained on the
average, by age 15.
5. Male musculature and body shape
By the end of puberty, adult men have heavier bones and nearly twice as much skeletal muscle.
6. Body odor and acne
Rising levels of androgens can change the fatty acid composition of perspiration, resulting in
a more "adult" body odor. Another androgen effect is increased secretion of oil (sebum) from
the skin and the resultant variable amounts of acne. Acne can not be prevented or diminished
easily, but it typically fully diminishes at the end of puberty.
2.29
Module
2:
Human
Reproductive
Anatomy
and
Physiology
|
Facilitator’s
Guide](https://image.slidesharecdn.com/fpcbt-level-1-for-facilitators-240228172608-b3930899/85/fpcbt-level-1-for-facilitators-pdf-for-the-Philippines-220-320.jpg)




















































![NARRATIVE
MODULE 4: INFECTION PREVENTION IN FP SERVICES
SESSION 2:INFECTION PREVENTION MEASURES
STANDARD PRECAUTIONS
Standard Precautions are designed for the safety and care of all people in a health care facility
– whether a hospitalized patient, a woman receiving IUD services, or a health care worker.
Because many people with blood-borne viral infections (i.e., hepatitis B [HBV] or C [HCV], HIV)
do not feel or look ill, standard precautions are to be applied consistently, regardless of the (known
or unknown) health status of those who are providing or receiving care.
When applied consistently, standard precautions act as protective barriers between
microorganisms and individuals, and are considered as highly effective means of preventing the
spread of infection.
The following considerations and actions help to form such barriers, as well as provide the means
for implementing the standard precaution:
• Consider every person (client or staff) as potentially infectious and susceptible to infection.
• Wash hands – the most important procedure for preventing cross-contamination (person to
person or contaminated object to person).
• Wear gloves (on both hands) before touching anything wet, broken skin, mucous membranes,
blood or other body fluids (secretions and excretions), soiled instruments, and contaminated
waste materials or for performing invasive procedures.
• Use physical barriers (protective goggles, face masks, and aprons) if splashes and spills of
blood or other body fluids are possible (e.g. when cleaning instruments and other items).
• Use antiseptic agents for cleansing skin or mucous membranes before surgery, cleaning
wounds, or doing hand rubs or surgical hand scrubs with an alcohol-based antiseptic product.
• Use safe work practices such as not recapping or bending needles, safely passing sharp
instruments, and suturing (when appropriate) with blunt needles.
• Safely dispose of infectious waste materials to protect those who handle them and prevent
injury or spread of infection to the community.
• Finally, process instruments, gloves, and other items after use by first decontaminating and
thoroughly cleaning them, and then either sterilizing or high-level disinfecting (HLD) them, using
recommended procedures. Again, in the context of IUD services, HLD is the recommended
method of final processing.
PROTECTIVE BARRIERS
Having a physical, mechanical or chemical "barrier" between microorganisms and an individual
(i.e., client, patient, and health worker) is an effective means of preventing the spread of disease.
The barrier serves to break the disease transmission cycle. Protective barriers are designed to
prevent the spread of infection from person to person, and from equipment, instruments, and
environmental surfaces to people and vice versa.
4.21
Module
4:
Infection
Prevention
In
Family
Planning
Services
|
Facilitator’s
Guide](https://image.slidesharecdn.com/fpcbt-level-1-for-facilitators-240228172608-b3930899/85/fpcbt-level-1-for-facilitators-pdf-for-the-Philippines-273-320.jpg)