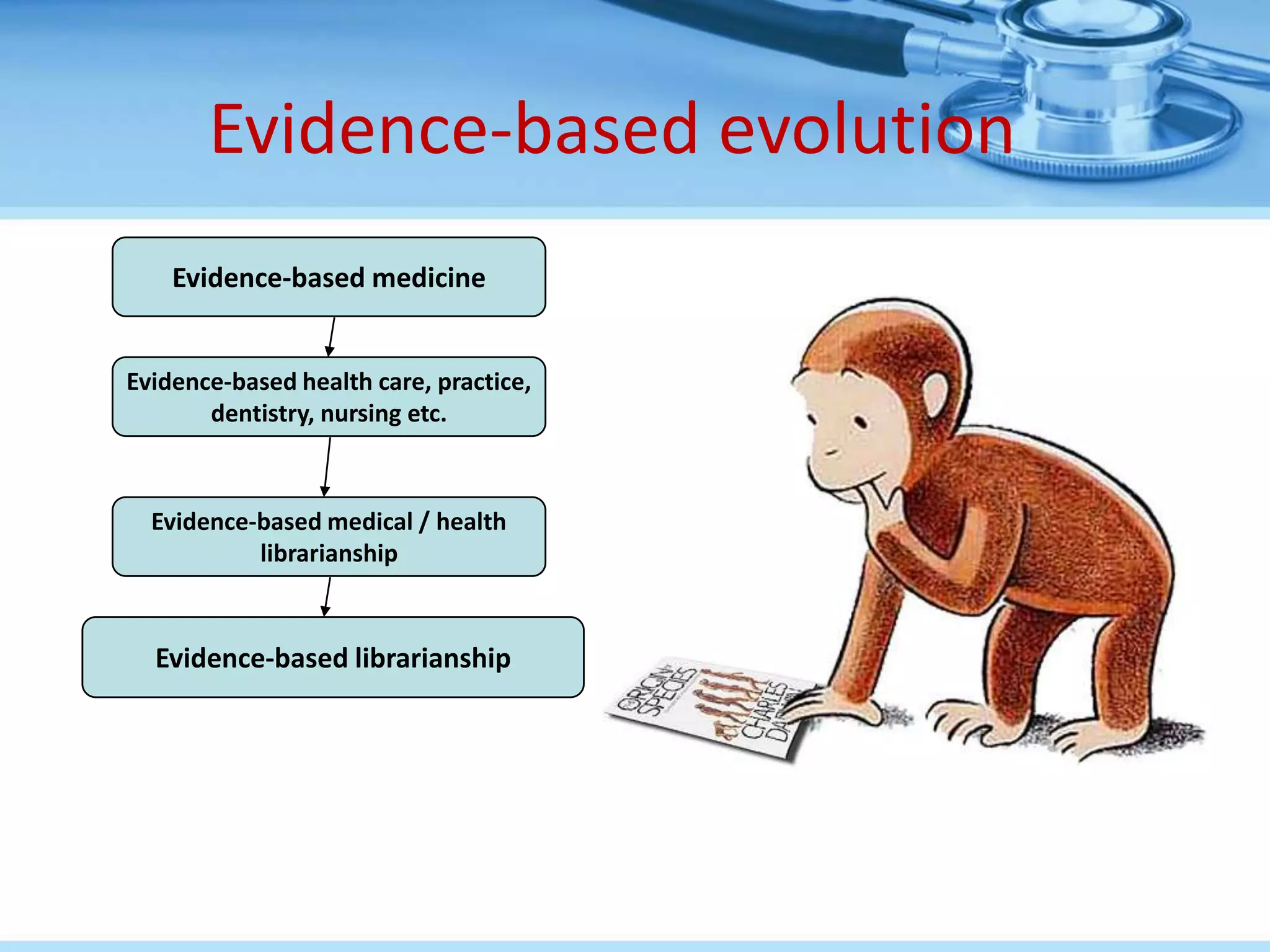
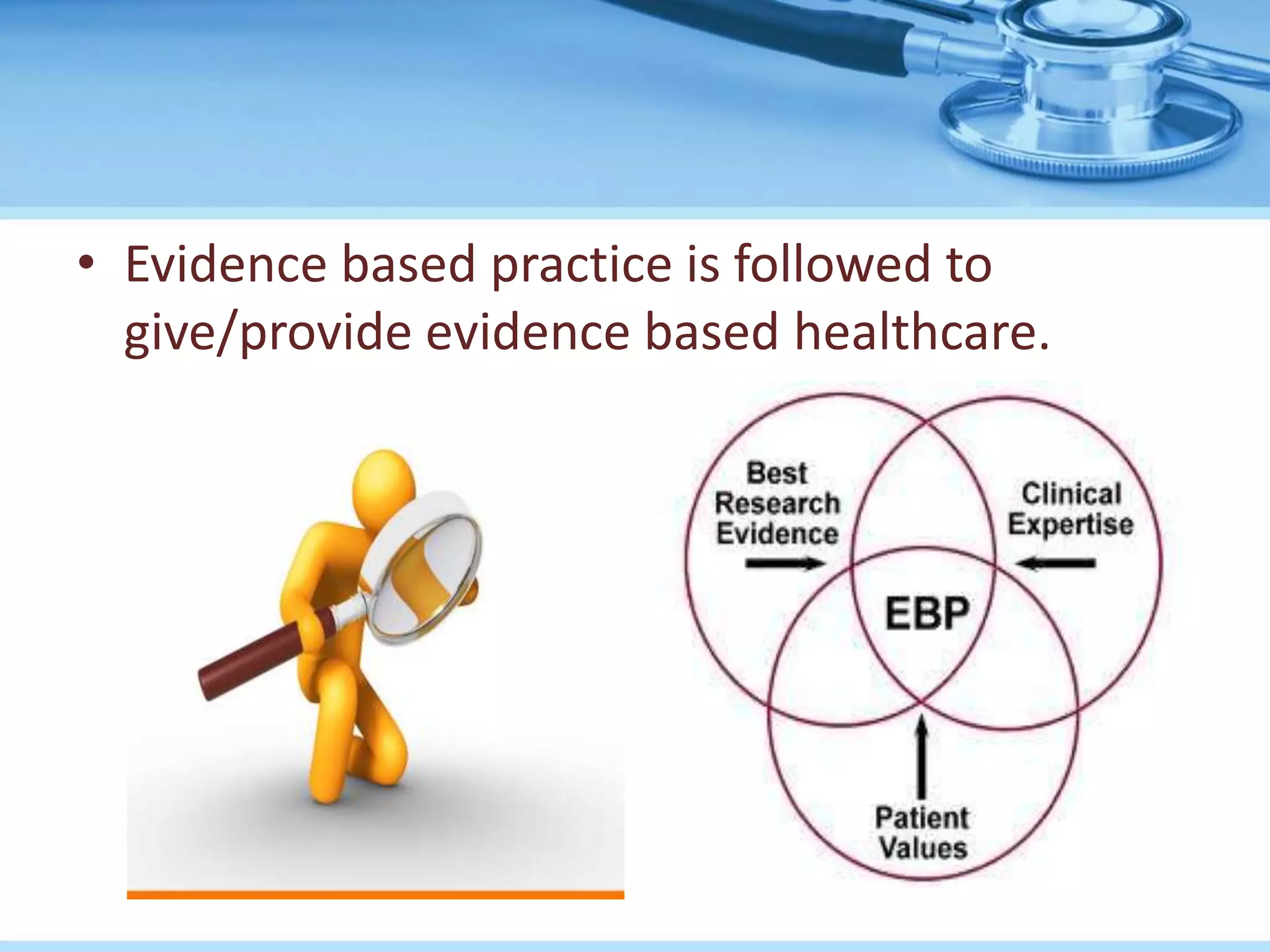
Evidence-based healthcare uses the best available clinical evidence from valid research combined with a health professional's expertise and experience to make decisions about patient care. It was introduced in 1991 to help clinicians incorporate research findings into their daily practice. Evidence-based healthcare aims to provide the highest quality of care using current best evidence from medical research on treatments, diagnostic tests, and other interventions. It involves forming clinical questions, searching literature, critically appraising evidence, and applying results to improve patient outcomes.