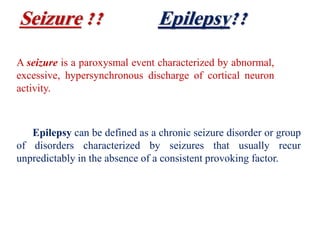
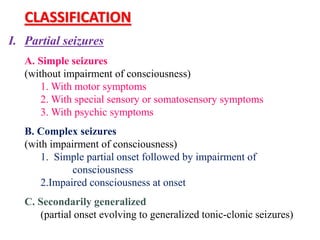
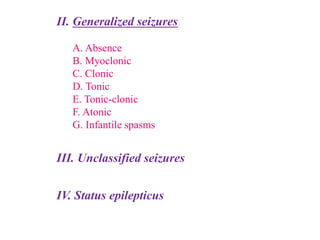
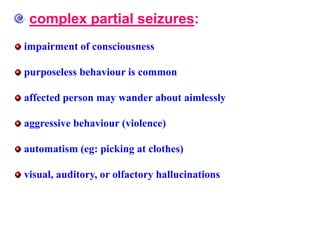
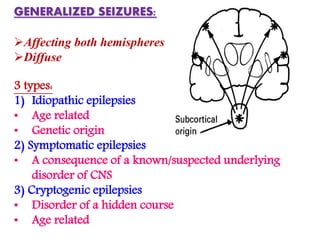
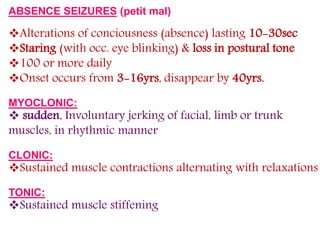
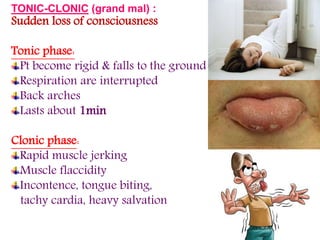
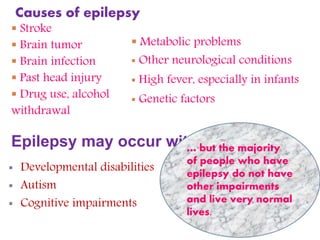
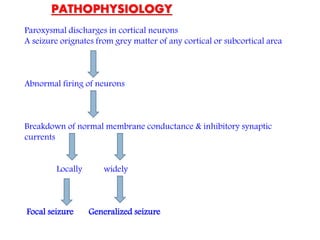
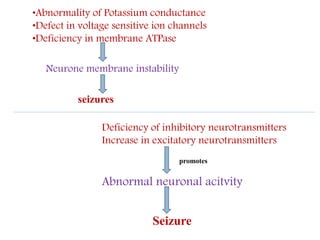
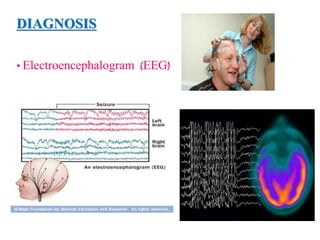
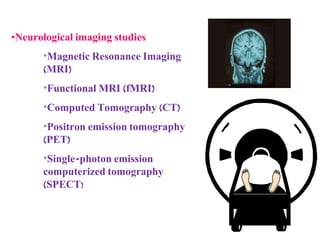
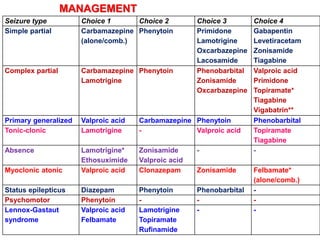
This document summarizes information about seizures and epilepsy. It defines a seizure as abnormal excessive neuronal discharge and epilepsy as a chronic seizure disorder. Seizures are classified as partial or generalized. Common causes of epilepsy include family history, head injuries, infections, and tumors. Diagnosis involves EEG and brain imaging. Treatment depends on seizure type but may include carbamazepine, lamotrigine, valproic acid, and other anticonvulsants. The majority of people with epilepsy live normal lives, as epilepsy is not contagious or a mental illness.