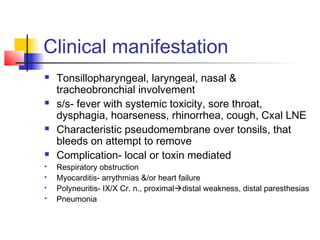
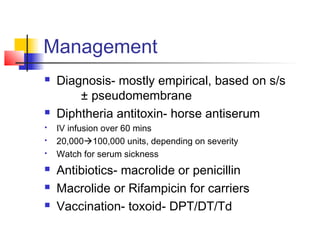
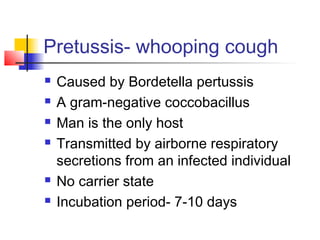
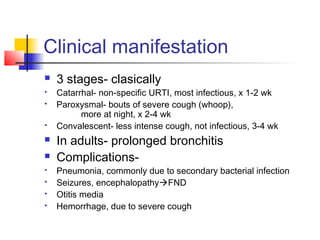
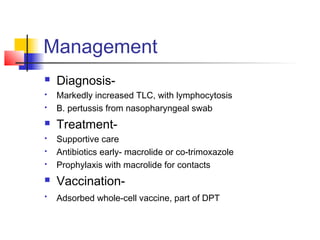
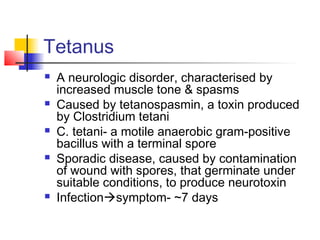
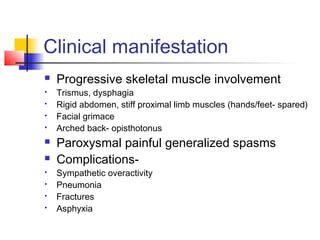
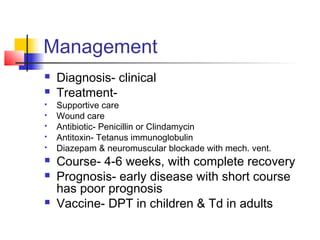
Diphtheria is caused by Corynebacterium diphtheriae and presents with a sore throat and formation of a gray membrane in the throat. Pertussis or whooping cough is caused by Bordetella pertussis and presents in three stages including coughing fits. Tetanus is caused by Clostridium tetani spores entering wounds and producing a neurotoxin resulting in painful muscle spasms. Vaccines exist to protect against all three diseases.