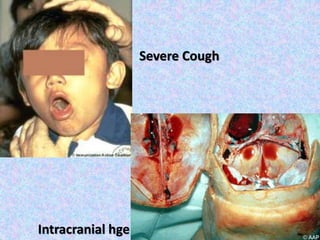
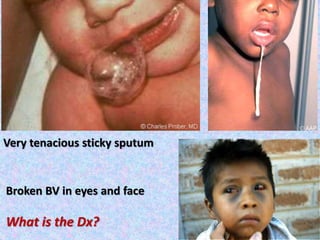
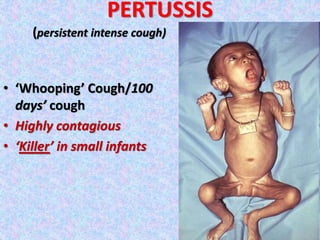
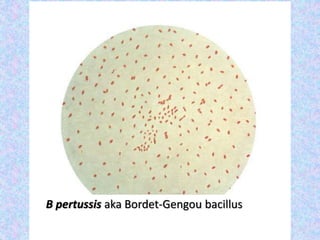
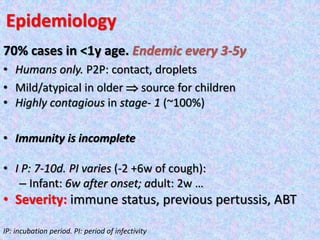
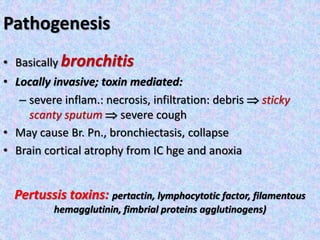
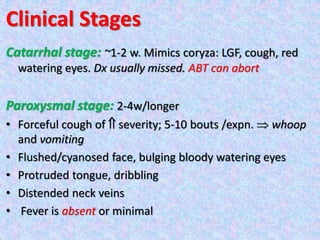
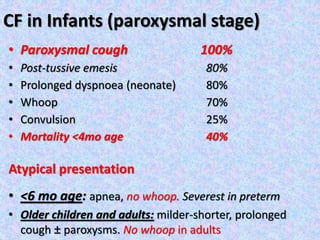
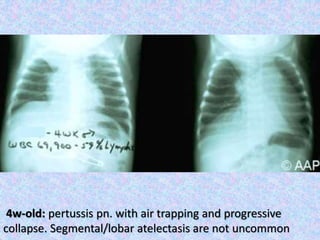
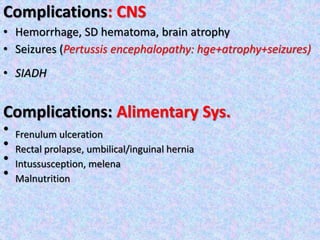
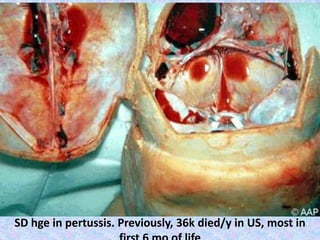
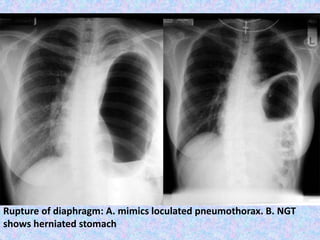
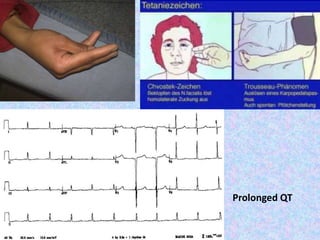
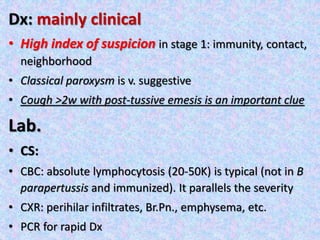
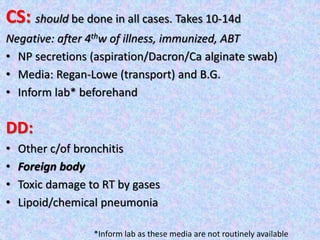
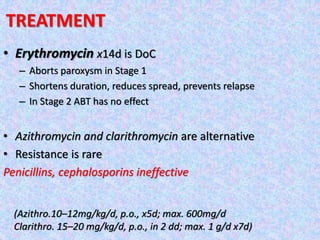
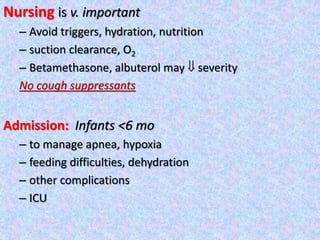
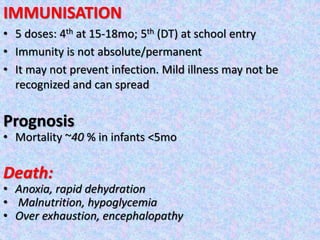
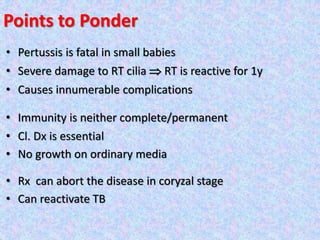
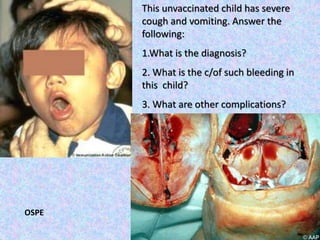
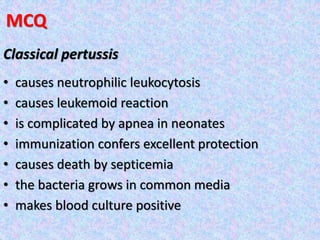
This document provides information about pertussis (whooping cough). It discusses the causative bacteria, Bordetella pertussis, and describes the typical three stages of the disease - catarrhal, paroxysmal, and convalescent. It notes the disease is highly contagious and a major killer of infants. Complications in infants can include pneumonia, seizures, and death. Diagnosis is usually clinical based on symptoms, and confirmed with lab tests. Antibiotics are the treatment of choice and aim to shorten the illness and prevent spread. Immunization provides protection but does not prevent all cases of pertussis.