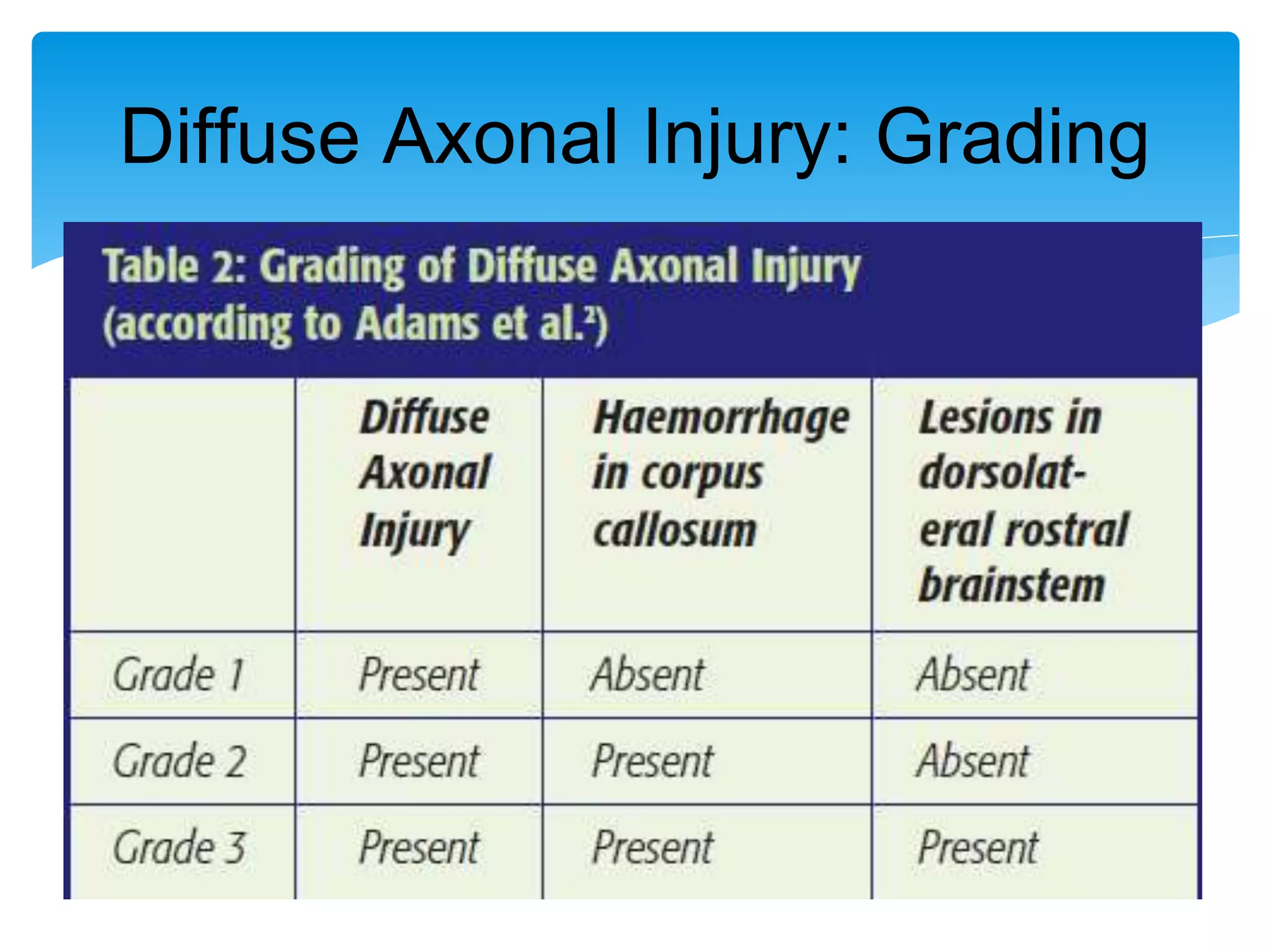
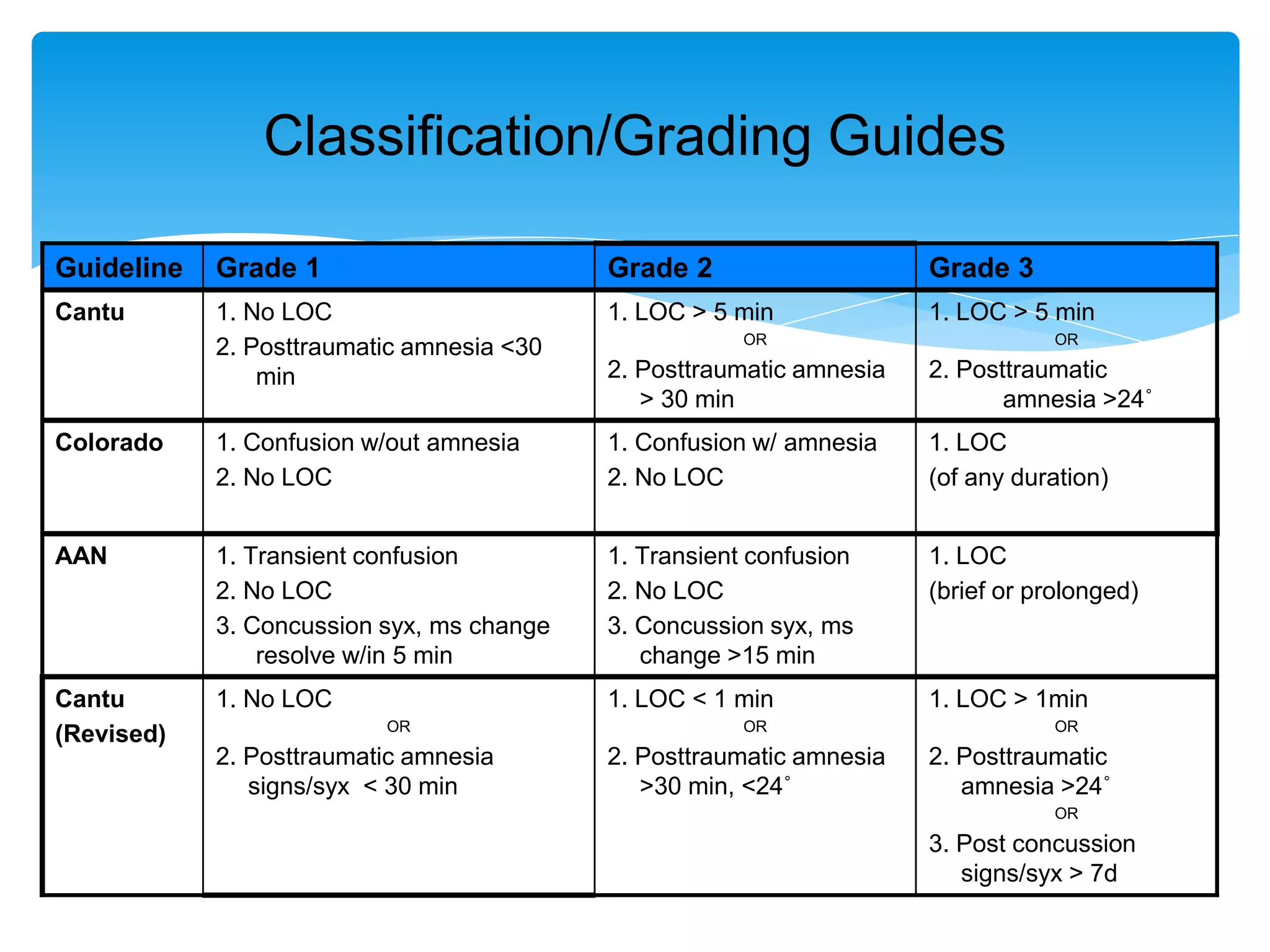
The document discusses diffuse axonal injury (DAI) and concussion, emphasizing that DAI is a significant cause of traumatic brain injuries in the U.S., primarily resulting from forces like acceleration/deceleration. Concussions, which may arise from various impacts, lead to temporary neurological impairments and can show no structural damage on imaging studies. The document also outlines classification and grading of concussions, management strategies, and long-term effects related to head injuries.