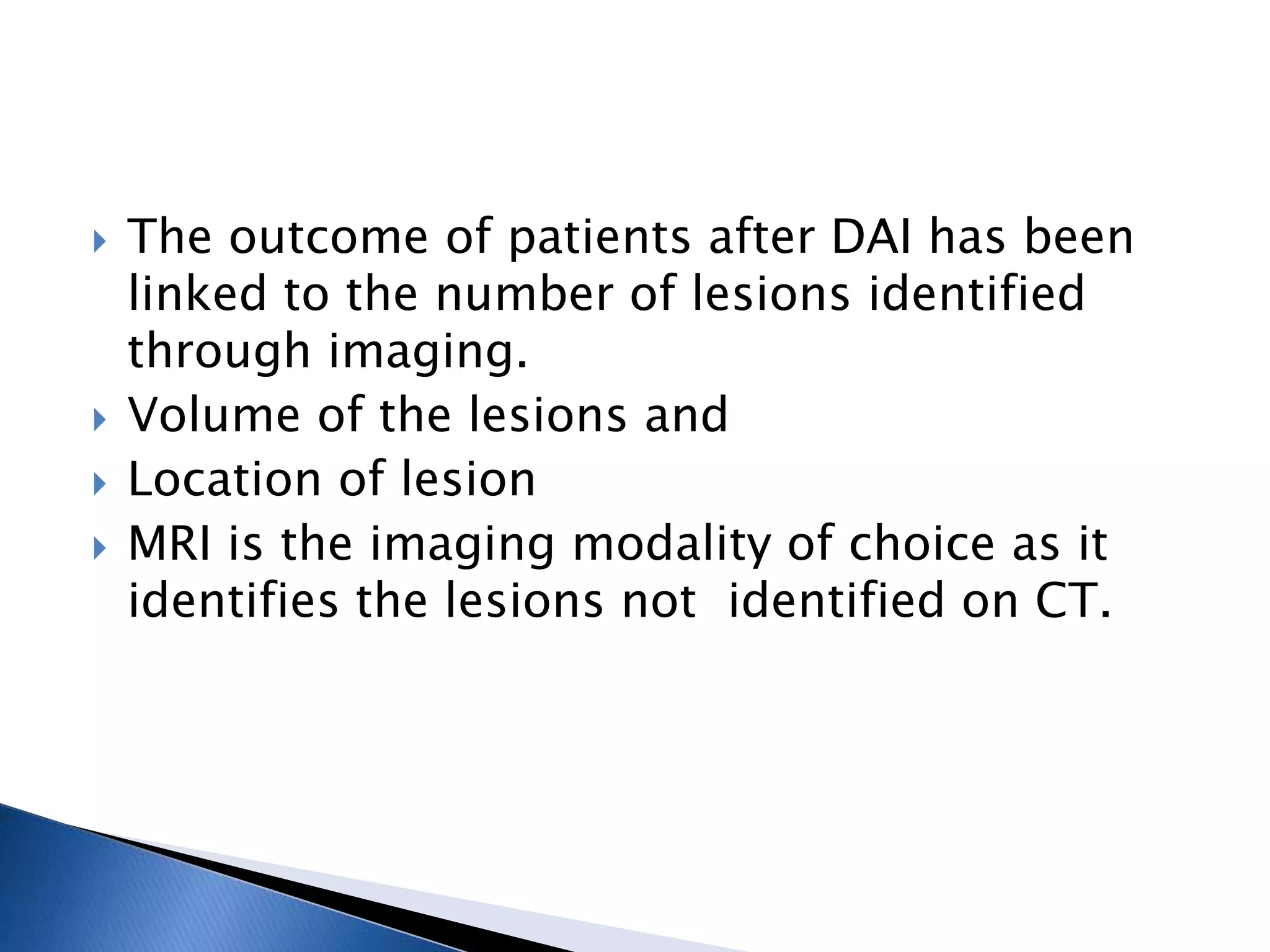
This document discusses diffuse axonal injury (DAI), a type of traumatic brain injury caused by shearing and tearing of axons. It occurs in about 50% of severe head injuries and can lead to loss of consciousness or a persistent vegetative state. The document outlines the pathogenesis and grading of DAI, as well as management strategies to prevent secondary brain injury like intracranial hypertension. Monitoring tools like intracranial pressure (ICP) measurement and multimodality monitoring are important for evaluation and guiding treatment.



![ Either following impact or from impulse
loading
Brain lags behind due to inertia
Movement away from skull cause low pressure
[ tensile strain] - contrecoup injuries
Strain within parenchyma cause diffuse injuries
[concussions and DAI], tissue tear
hemorrhages.](https://image.slidesharecdn.com/dai-200312225617/75/Diffuse-axonal-injury-6-2048.jpg)



![Grading of DAI: [ Gennarelli et al 1982]
I. Microscopic axonal damage in the white matter, corpus
callosum, brain stem or cerebellum without any macroscopic
evidence.
II. Macroscopic or Microscopic detected focal lesions in the
CC and diffuse axonal damage.
III. Macroscopic or microscopic injury, focal injury to CC +
dorsolateral quadrant of rostral brain stem.](https://image.slidesharecdn.com/dai-200312225617/75/Diffuse-axonal-injury-12-2048.jpg)