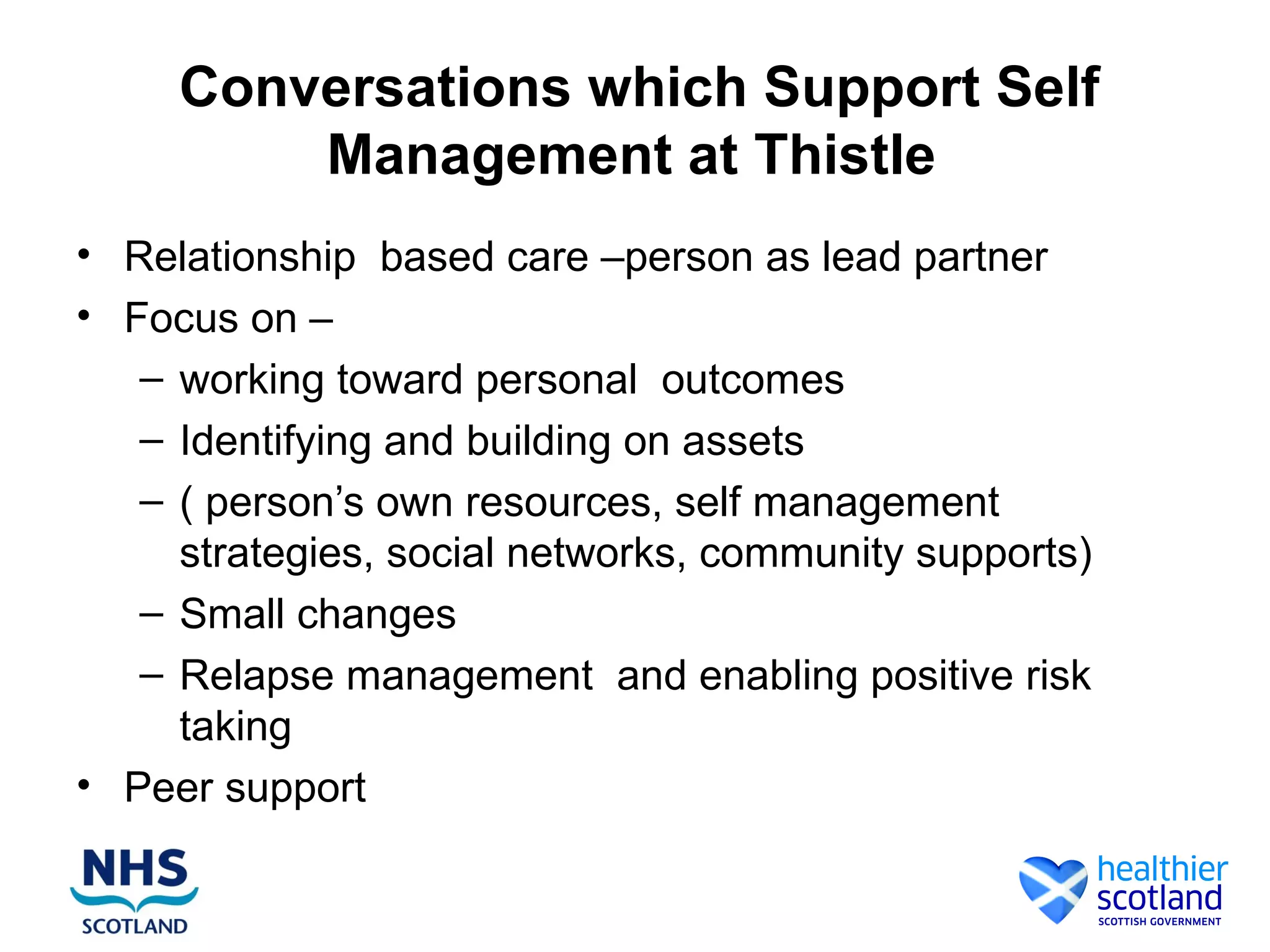
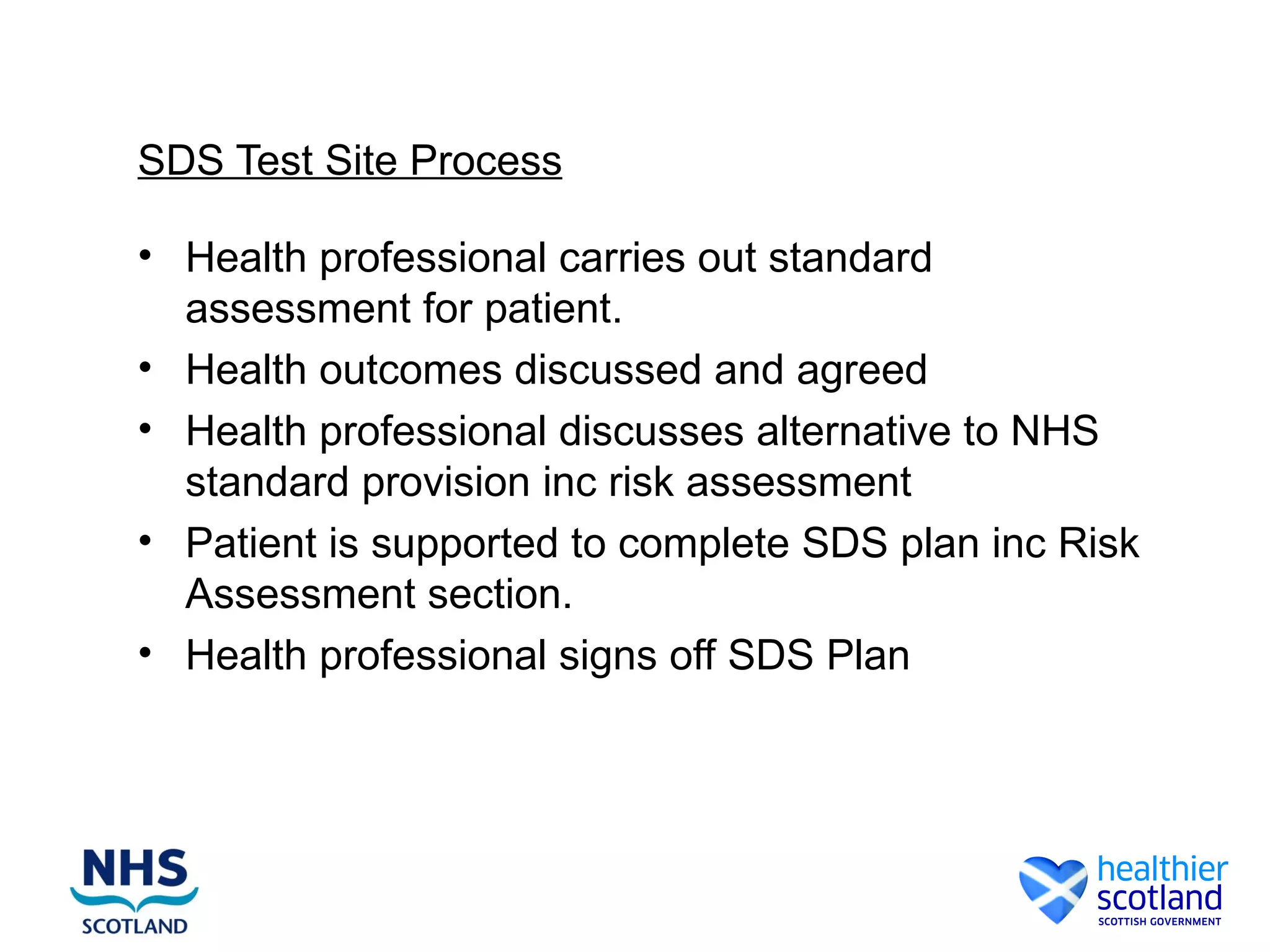
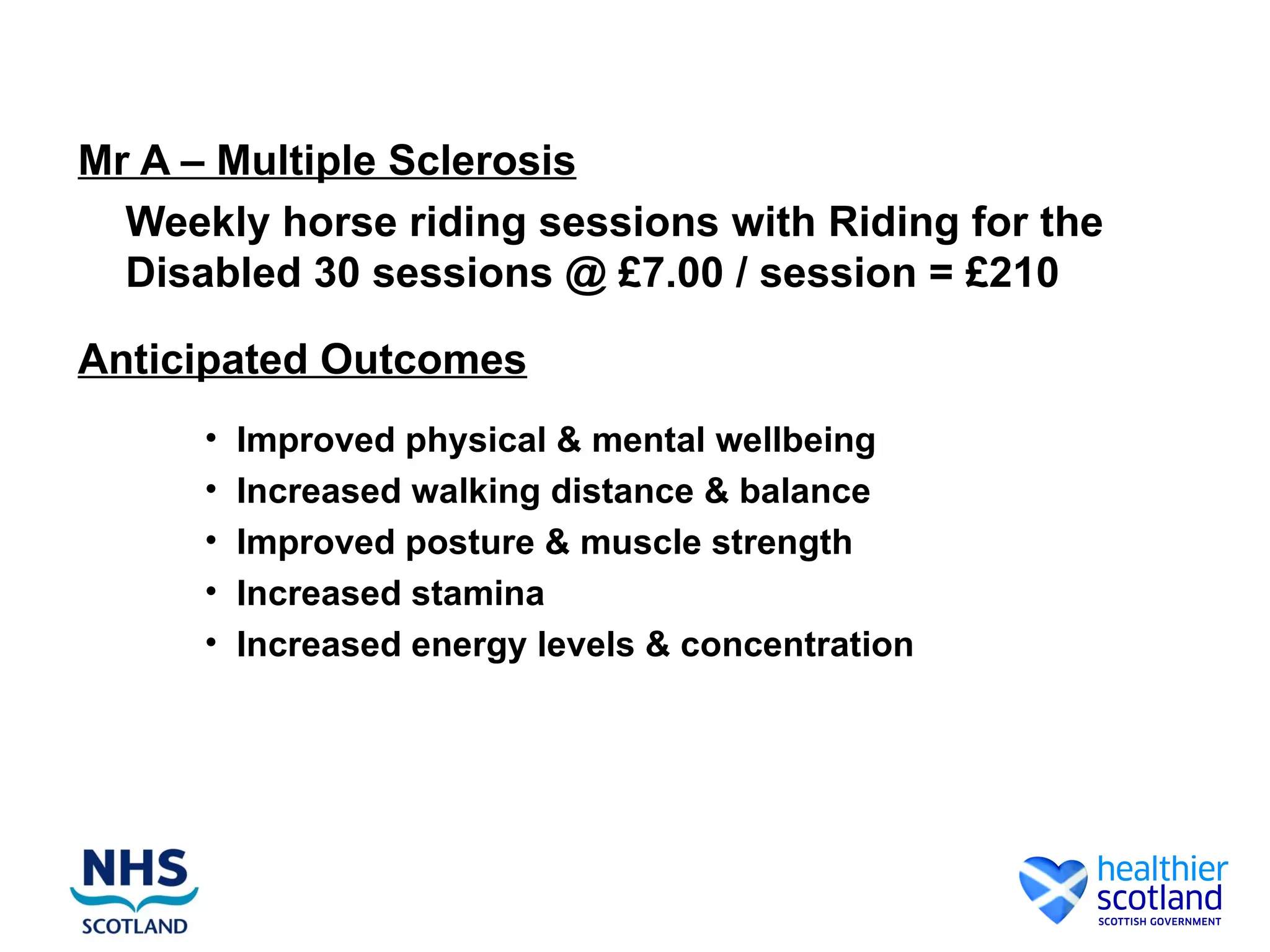
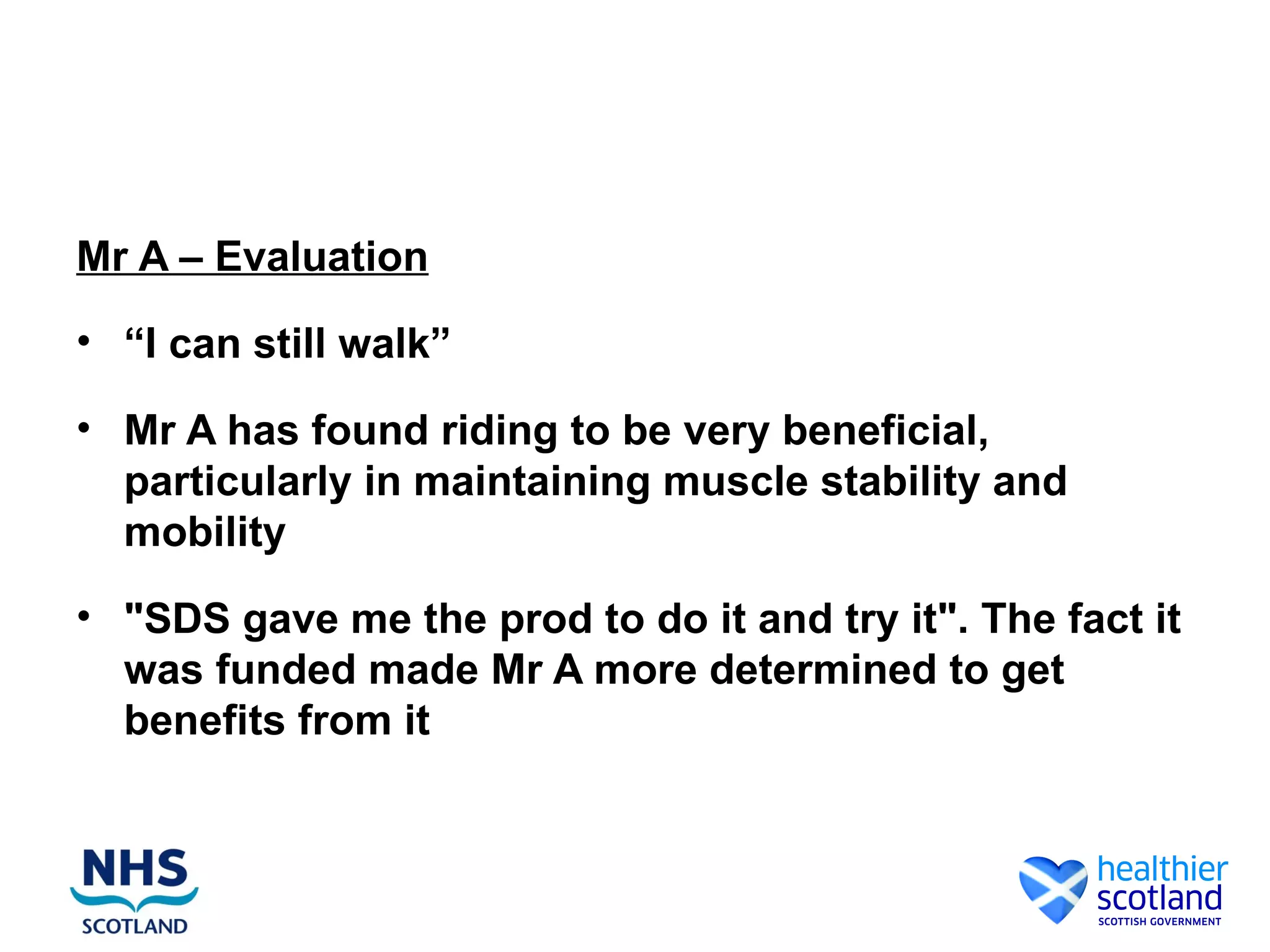
The document discusses creative and innovative approaches to empowering people through self-management and greater control over their health outcomes and risks. It focuses on person-centered care, identifying assets and building support networks to facilitate self-management of long-term conditions. The importance of risk enablement is emphasized to promote choice and control for individuals through self-directed support options.