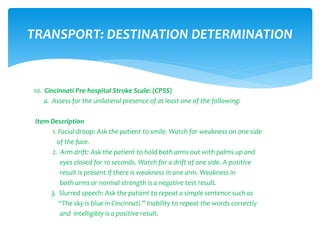
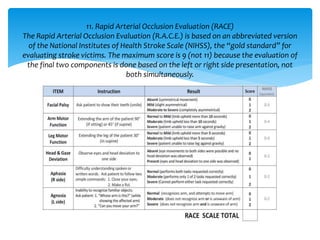
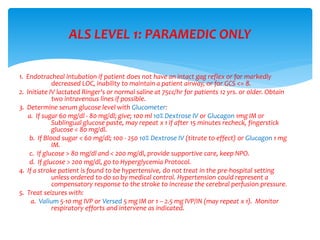
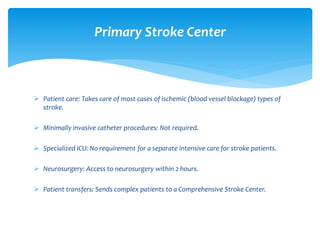
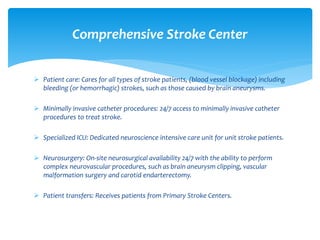
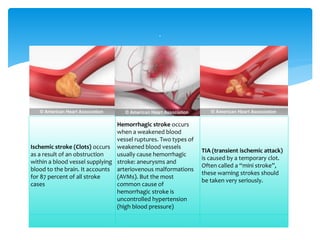
The document provides information about protocols for treating patients exhibiting signs of an acute stroke or CVA. It outlines assessments and tests to determine if a patient is having a stroke, including the Cincinnati Pre-hospital Stroke Scale (CPSS) and Rapid Arterial Occlusion Evaluation (RACE). It describes treating potential underlying causes of stroke symptoms like hypoglycemia. It also notes the differences between primary and comprehensive stroke centers in terms of capabilities for treating patients.