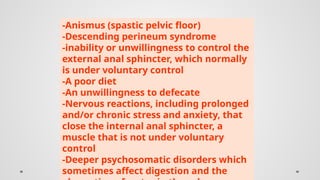
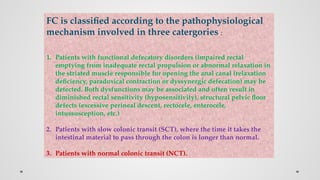
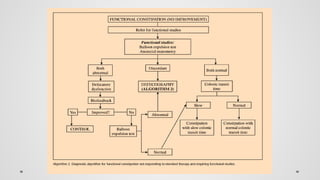
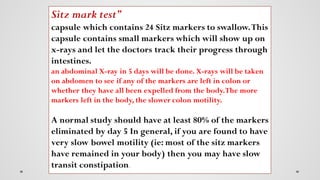
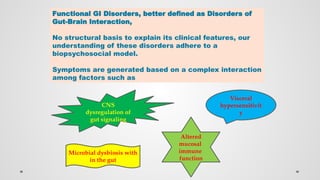
The document provides a comprehensive overview of constipation, including its definition, risk factors, common causes, and distinctions between functional constipation and irritable bowel syndrome (IBS). It elaborates on diagnostic criteria, necessary tests, and treatment strategies, particularly for chronic idiopathic constipation. Treatment options discussed include dietary measures, biofeedback therapy, and pharmacological interventions such as plecanatide.








![: Patient reports that abnormal bowel
movements are usually constipation (like
type 1 or 2 in the picture of Bristol Stool
Form Scale [BSFS]](https://image.slidesharecdn.com/constipation-250127192850-6b7e404e/85/CONSTIPATION-pptx-11-320.jpg)