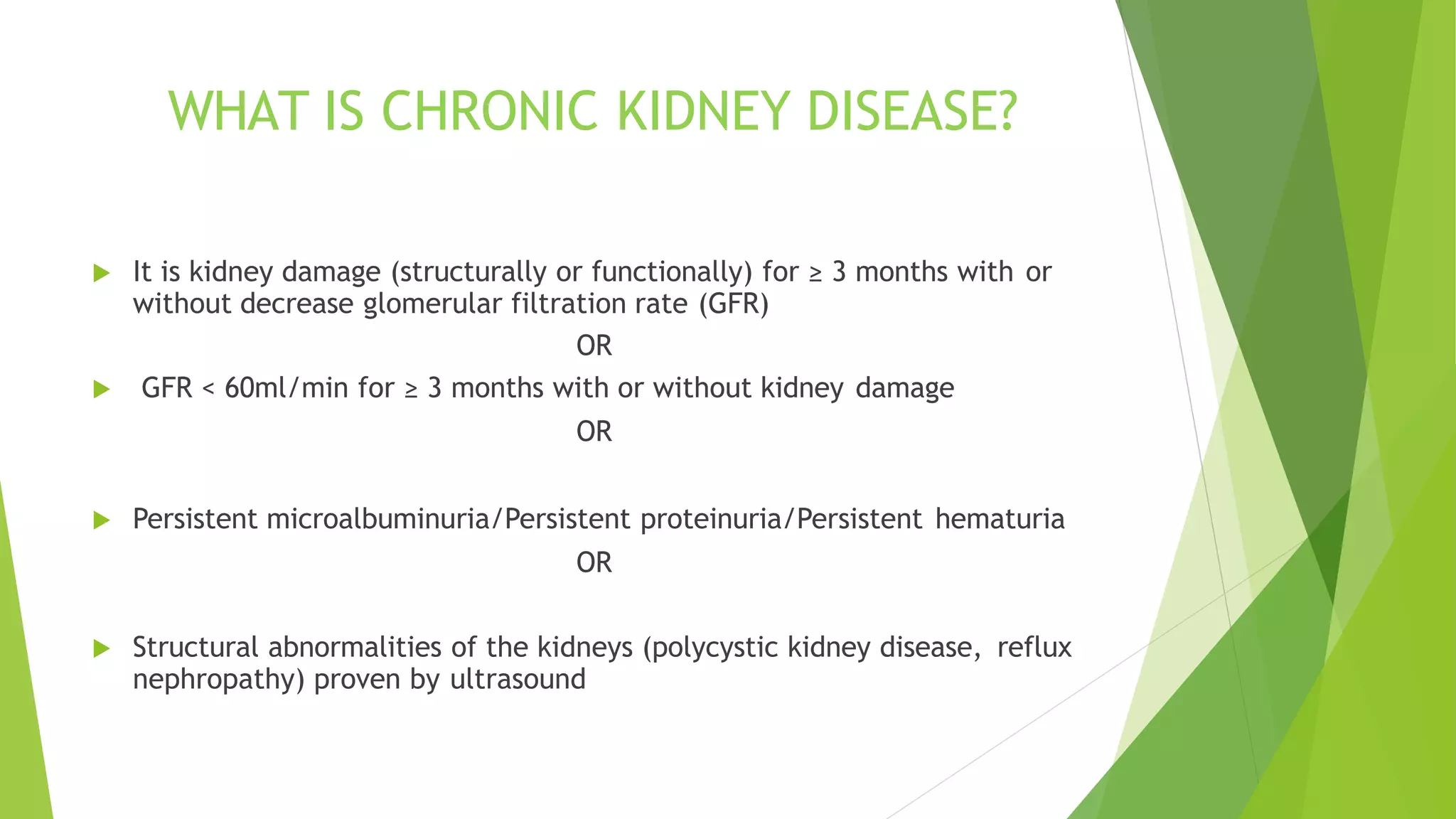
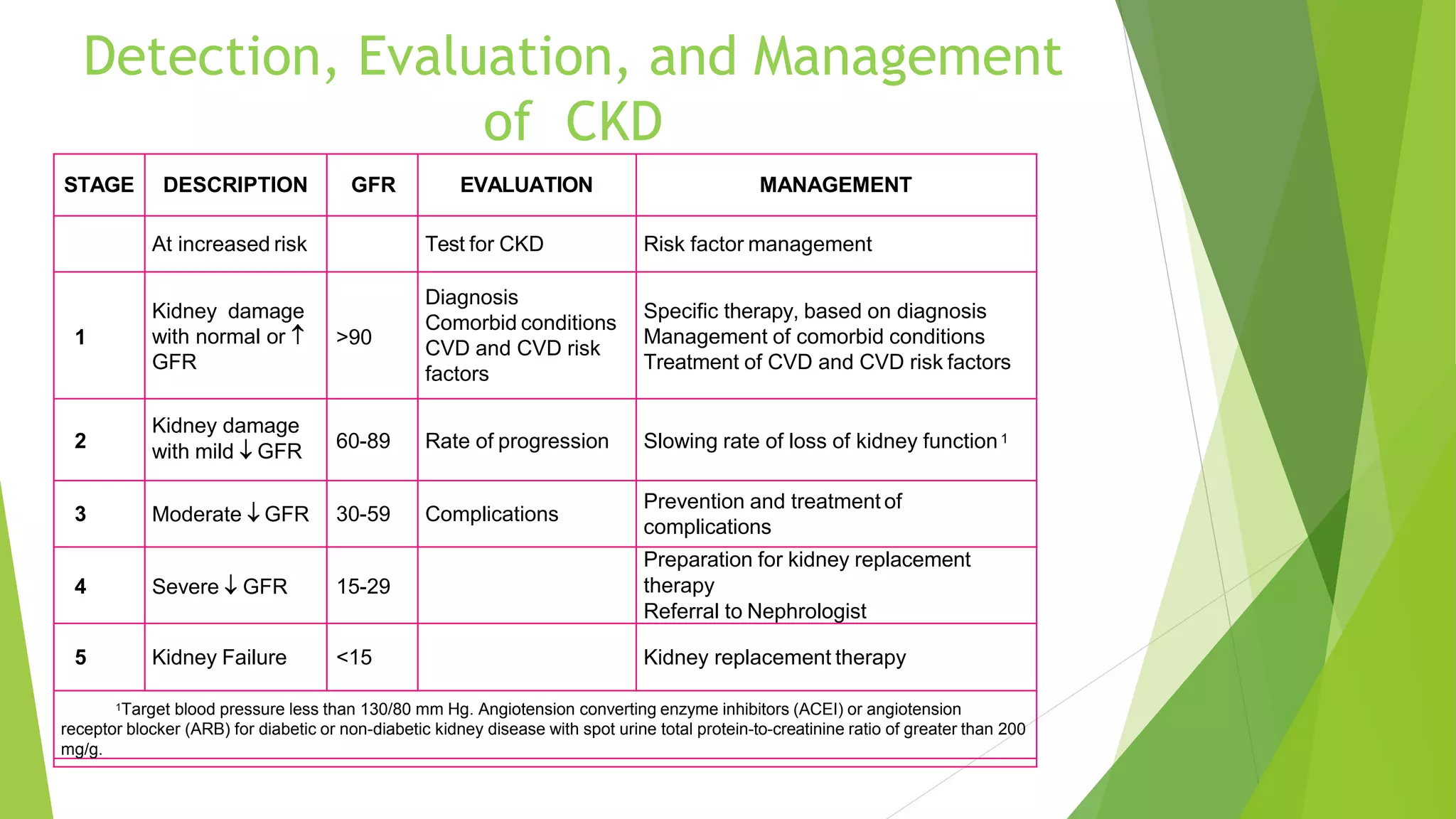
This document provides an overview of the management of chronic kidney disease (CKD). It defines CKD and describes its most common causes as diabetes mellitus and hypertension. It explains the pathophysiology of CKD as progressive loss of nephrons leading to activation of the renin-angiotensin-aldosterone system and hypertension. The clinical presentation ranges from asymptomatic early on to later symptoms of kidney failure like fluid overload and hyperuremia. Diagnosis involves assessing glomerular filtration rate and looking for signs of kidney damage through blood and urine tests. Treatment aims to control blood pressure and glucose, treat underlying causes, and prevent complications through diet, medications, and renal replacement therapy like dialysis if indicated. Complications discussed