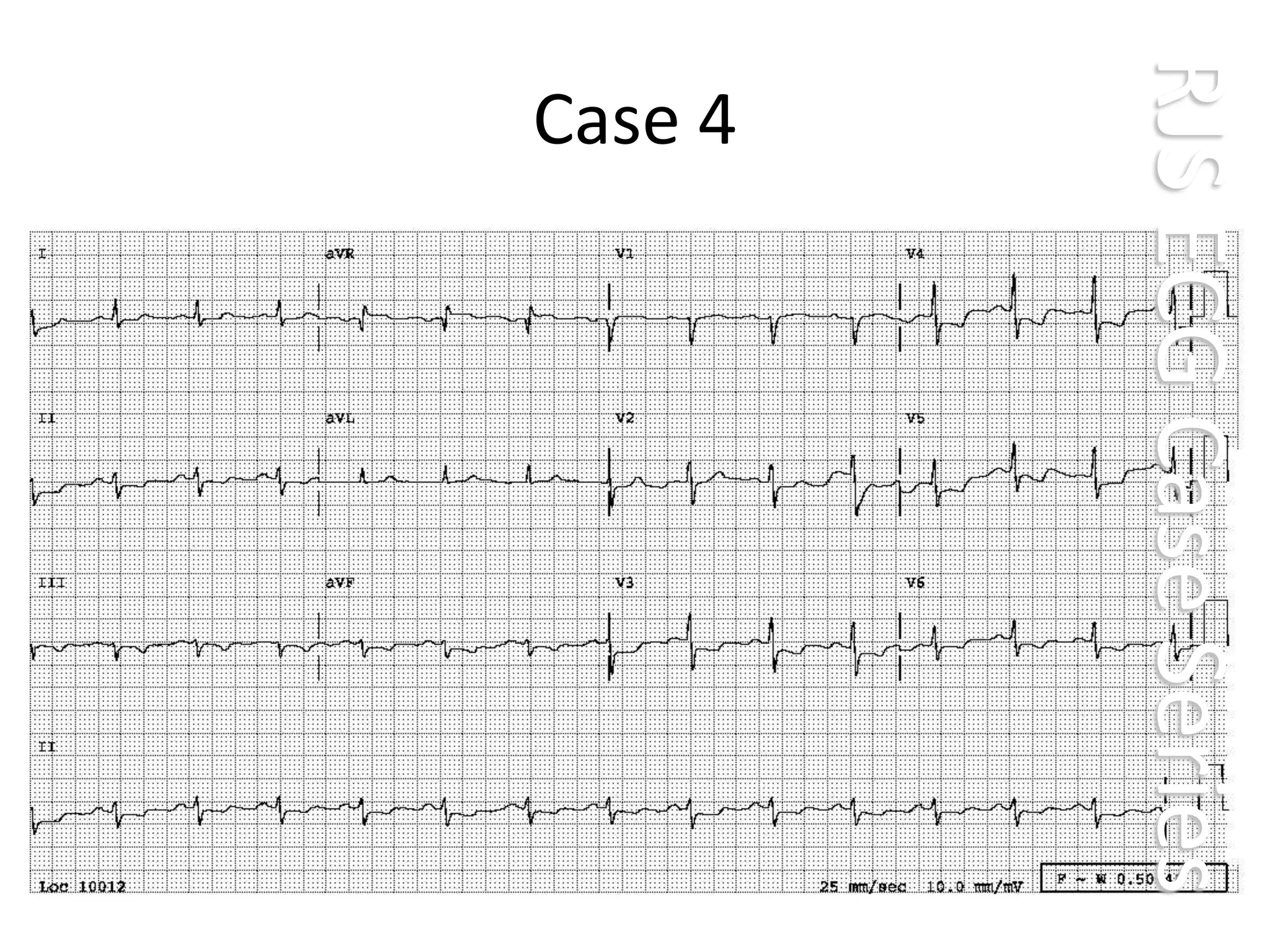
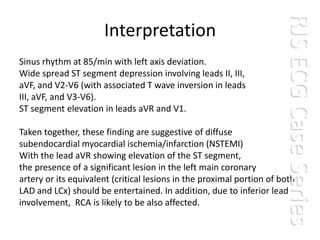
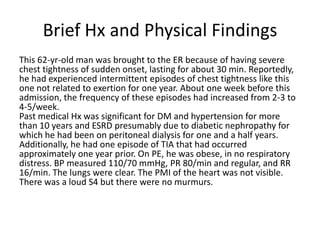
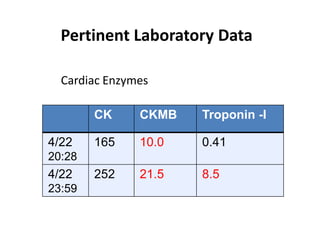
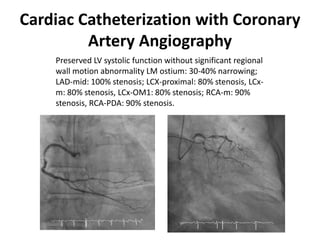
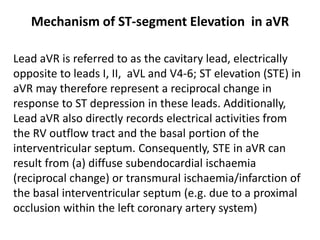
This ECG shows signs of diffuse subendocardial ischemia/infarction in a 62-year-old man with chest tightness and risk factors of diabetes, hypertension, and kidney disease. The ECG findings include left axis deviation, ST segment depression in multiple leads, and ST elevation in leads aVR and V1, suggesting involvement of the left main coronary artery or proximal LAD and LCx arteries. Cardiac enzymes were elevated. Coronary angiography revealed significant stenoses of the left main, LAD, LCx, and RCA arteries consistent with triple vessel disease.